Pathology
An acute coronary syndrome refers to any process where heart muscle receives less oxygen than it needs. It encompasses three separate, but overlapping pathologies: unstable angina, non-ST elevation myocardial infarction (NSTEMI), and ST elevation myocardial infarction (STEMI). Therefore, acute coronary syndrome represents a continuum of severity, which if severe enough, can lead to irreversible cardiac muscle death.
NSTEMI and STEMI are distinguished from unstable angina by the presence of heart muscle death. NSTEMI occurs when the inner most portion of the heart wall dies, and is generally due to a partially occlusive thrombus (blood clot) in one of the coronary arteries or their branches. An NSTEMI can, in some ways, be thought of as a "partial" heart attack.
On the other hand, STEMI occurs when a coronary blood vessel becomes fully blocked by thrombus. If untreated, the result is transmural (full wall) death of the heart muscle that the occluded vessel serves. A STEMI, in non-technical terms, can be thought of as a "full blown" heart attack.
Coronary thrombi (blood clots) form after rupture of an atherosclerotic plaque. The exposed plaque surface is highly thrombogenic, which means that blood clots form easily on it. The exposed surface causes platelet and coagulation cascade activation, which results in a thrombus that can occlude the entire vessel diameter resulting in decreased, or in the worst case scenario, no blood flow to the heart muscle. This is the basis of a "heart attack" or myocardial "infarction".
Signs, Symptoms, and Complications
Symptoms of acute coronary syndrome are consistent with anginal chest pain. If angina occurs at rest, or with less activity than it normally does, this is referred to as "unstable" angina, and signifies increased narrowing (ie: decreased diameter) of a coronary blood vessel.
Substernal “crushing” chest pain is the classic description of a heart attack (either NSTEMI or STEMI) and is usually accompanied by diaphoresis (ie: excessive sweating). In addition, nausea and vomiting can also occur. Pain from the chest can sometimes radiate into the arm (usually the left arm) or the jaw. Numbness and tingling in the arm and jaw are also common features. Shortness of breath is another symptom of heart attack, and is usually due to the acute back up of blood into the vessels of the lung, which leads to pulmonary edema.
Complications of infarction are due to mechanical changes in the heart. Damage of the electrical conduction system can lead to arrhythmias (abnormal heart rhythms), which are common in the first few days after an infarction.
If enough heart muscle is destroyed cardiogenic shock can occur. This happens when the heart is no longer able to pump enough blood to the rest of the body. Decreased blood flow to the other organs can lead to ischemia of these organs and multi-organ failure.
and "heart attack"
refer to the same thing –
death of heart muscle.
Finally pericarditis, or inflammation of the sack that the heart sits in, can also occur. A condition known as Dressler’s syndrome is pericarditis that occurs after a heart attack. It usually occurs two weeks to several months after the infarction.
Long term complications of myocardial infarction include heart failure. Ultimately the damaged heart is unable to beat as well as it did in the past. This leads to the back up of blood and fluid in the lungs causing shortness of breath, amongst other symptoms.
Diagnosis
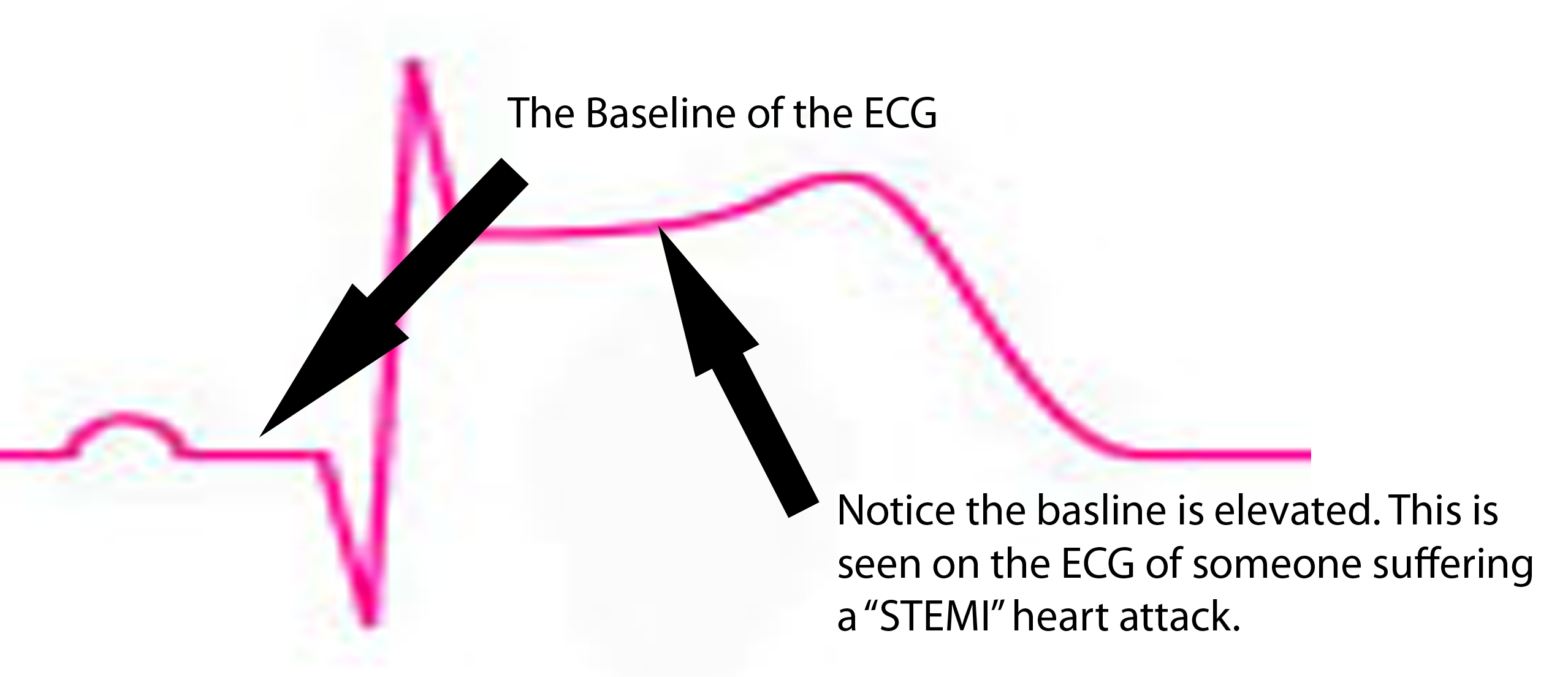
Diagnostic studies can confirm NSTEMI or STEMI. An electrocardiogram (ECG) is the gold standard. It will show ST segment depression in NSTEMI, and ST segment elevation in STEMI. Q-waves are also seen, but may represent previous infarction.
Blood tests can also show elevations in specific proteins released by the dying heart muscle. Cardiac troponin I is one of these markers, and is the most specific for heart muscle injury. It begins to rise 4 hours after the initial thrombus formation and stays elevated for 7-10 days. CK-MB (creatine kinase myocardial band) is another protein released by damaged heart tissue; it is useful in that it is cleared relatively quickly compared to troponin; this is useful in that it can aid in detection of early re-infarction.
Image (right) – An ECG of someone with an NSTEMI. Notice how the 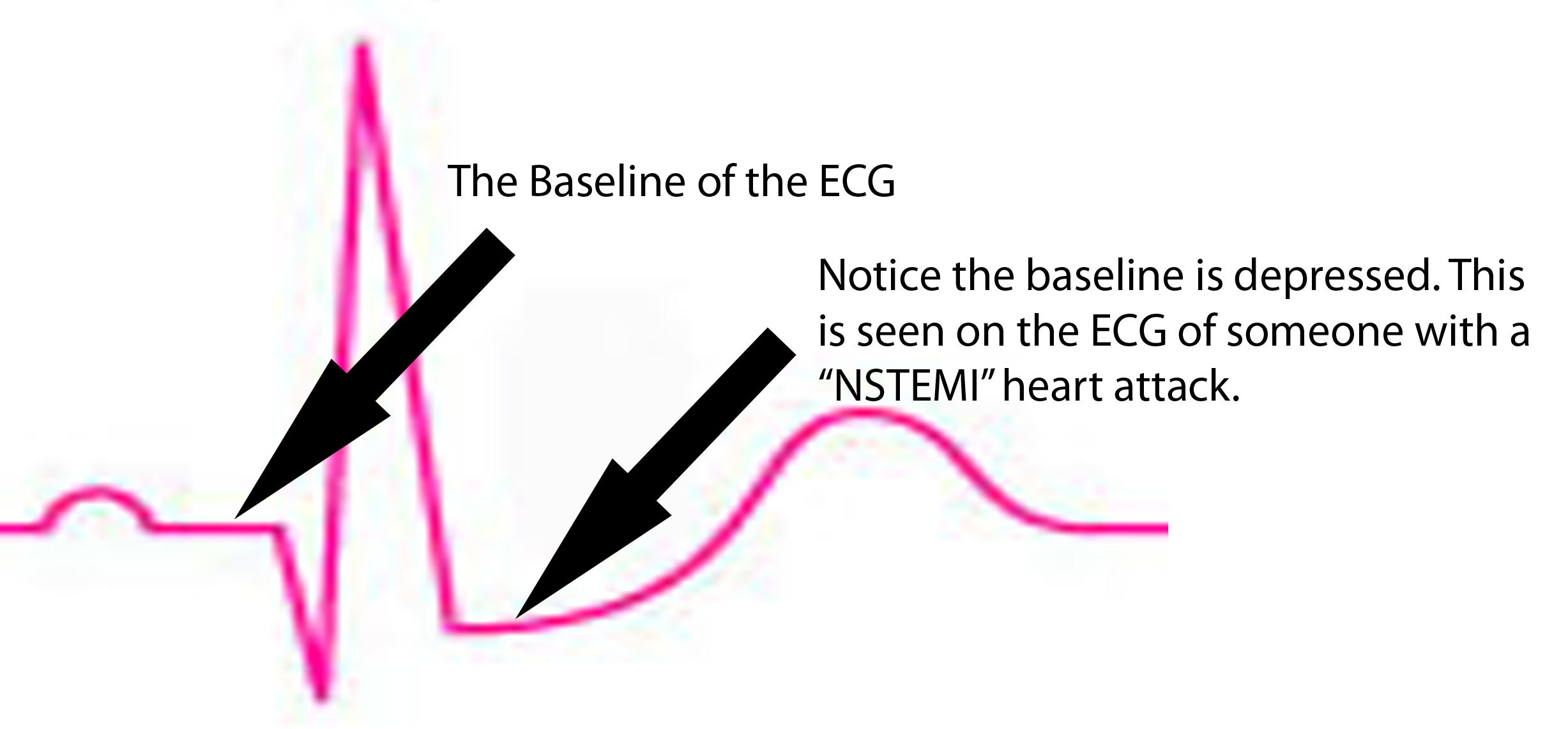 ST segment is depressed below baseline.
ST segment is depressed below baseline.
Treatment
The main goals of treatment are to restore blood flow, and to decrease the amount of work the heart is doing. Both of these measures help provide oxygen to the dying heart muscle. One of the main problems in myocardial infarction is that the heart is working harder than usual, and is doing so under decreased oxygen delivery (ie: decreased blood flow). This deadly combination increases the rate of heart muscle death. Therefore, treatment is designed to increase oxygen flow (ie: by restoring blood flow), or by decreasing the work of the heart, and therefore the amount of oxygen the heart needs to survive.
Treatment of any patient with suspected acute coronary syndrome should include pain control. For example, morphine controls the pain associated with heart attacks, and this indirectly lowers the heart rate. Lowering the heart rate decreases the amount of work the heart muscle is doing, and therefore decreases the amount of oxygen that must be delivered for muscle survival.
In addition, nitroglycerin is given because it decreases preload. Preload refers to the amount of blood inside the left ventricle just before contraction of the heart. A larger preload means that the heart must work harder because, in essence, it is pumping more blood per beat. Nitroglycerin dilates blood vessels (mostly veins) in the body and effectively decreases the amount of blood within the heart itself. Less blood to pump, equals less work the heart must do.
Oxygen therapy should also be started to help improve blood oxygen levels. This will ensure that any blood getting to the myocardium will have as much oxygen as possible.
There are several methods for restoring blood flow. The preferred method is through percutaneous coronary interventions (PCI). In this procedure a small catheter is inserted into blood vessels in the groin and threaded up towards the heart; once in the blood vessels of the heart the catheter can be used to mechanically remove any blockage. This is known as "angioplasty" or "thrombectomy". Percutaneous coronary intervention should occur in a reasonable amount of time. There is debate about the exact timing and depends on the type of acute coronary syndrome (ie: STEMI vs NSTEMI).
If the hospital does not have the capacity to do PCI then medications can be used to "break up" the blood clot/thrombus. All patients with suspected infarction should receive an aspirin. Aspirin works by inhibiting platelet plug formation. This helps slow the rate of thrombus formation. First line medications for restoring flow in myocardial infarction are intravenous unfractionated heparin or subcutaneous enoxaparin. Fibrinolytics like tissue plasminogen activator (tPa), reteplase, streptokinase, and urokinase are also sometimes used to try and restore blood flow.
Finally, revascularization operations (ie: coronary artery bypass grafting) may also be necessary depending on the level of disease in the other coronary vessels.
Overview
Acute coronary syndrome refers to a continuum of coronary blood vessel blockage. On the least extreme end is unstable angina; on the most extreme (ie: most dangerous) end is ST elevation myocardial infarction. Symptoms are usually crushing chest pain that radiates to the jaw and arm, but may also include nausea, vomiting, dizziness/fainting, and sweating. Diagnosis is based of ECG and blood tests for heart muscle damage. Treatment is aimed at increasing blood flow, and therefore oxygen delivery, to the heart muscle. This is done by decreasing the amount of work the heart is doing, increasing the amount of oxygen present in blood, and breaking up the blood clot via mechanical or medical means.
References and Resources
- Husted SE, Nielsen HK. Unfractionated heparin and low molecular weight heparin for acute coronary syndromes–assessment of a Cochrane review. Ugeskr Laeger. 2010 Sep 13;172(37):2522-6.
- Lepor NE, McCullough PA. Differential diagnosis and overlap of acute chest discomfort and dyspnea in the emergency department. Rev Cardiovasc Med. 2010;11 Suppl 2:S13-23. >
- Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. Seventh Edition. Philadelphia: Elsevier Saunders, 2004. >
- Lilly LS, et al. Pathophysiology of Heart Disease: A Collaborative Project of Medical Students and Faculty. Fourth Edition. Lippincott Williams and Wilkins, 2006.
- Flynn JA. Oxford American Handbook of Clinical Medicine (Oxford American Handbooks of Medicine). First Edition. Oxford University Press, 2007.
- Ferguson JJ, Califf RM, Antman EM, et al. Enoxaparin vs unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes managed with an intended early invasive strategy: primary results of the SYNERGY randomized trial. JAMA. 2004 Jul 7;292(1):45-54.