Relative Value Units (RVUs) have been utilized in the United States healthcare system for several decades as a standardized method for quantifying the “value” of medical services. They have become an important component of determining physician reimbursement. While the RVU system was initially designed to bring uniformity and transparency to physician payments, it has been increasingly criticized for its shortcomings in accurately reflecting physician worth. This article will discuss the key reasons why RVUs are a flawed measure of physician worth and explore alternative methods of evaluation.
Focus on Quantity over Quality
One of the most significant criticisms of the RVU system is its emphasis on the volume of services provided rather than the quality of care. By assigning higher RVU values to more complex and time-consuming procedures, the system inadvertently incentivizes physicians to prioritize high-revenue-generating procedures over less profitable, but potentially necessary, patient care activities. This focus on quantity can compromise the quality of care and hinder a physician’s ability to provide patient-centered care.
Lack of Personalized Care
RVUs are based on standardized averages, which do not account for individual variations in patient needs, physician skill, and the complexity of cases. Consequently, the RVU system fails to recognize the nuances of personalized care that physicians provide. High-quality care often involves tailoring treatment plans to each patient’s unique circumstances, which may not align with the fixed values assigned by RVUs. For example, if a primary care physician spends an entire hour discussing a patient’s mental health issues in a caring and compassionate way they are reimbursed substantially less than an orthopedic surgeon who takes an hour to pin a fracture or a neurosurgeon who spends an hour doing a cervical discectomy and fusion.
Limited Scope of Measurement
The RVU system only captures a narrow scope of a physician’s worth by focusing solely on clinical procedures and services. It does not account for the many other essential aspects of healthcare, such as patient education, interdisciplinary collaboration, care coordination, and research contributions. By overlooking these non-clinical activities, the RVU system fails to provide a comprehensive evaluation of a physician’s value.
Inadequate Incentive for Preventative Care
Preventative care plays a critical role in promoting public health and reducing healthcare costs. However, the RVU system does not adequately incentivize physicians to engage in these activities, as they are generally assigned lower RVUs. This discrepancy may lead to an underemphasis on preventative care and a potential increase in long-term healthcare costs.
Perpetuation of Disparities
RVUs can contribute to healthcare disparities by allocating resources based on service volume rather than patient need. Physicians practicing in underserved areas may find it challenging to generate high RVU values due to lower patient volume or a greater focus on primary care. This imbalance in resource distribution may inadvertently widen the gap in healthcare access and quality.
Lack of Collegiality
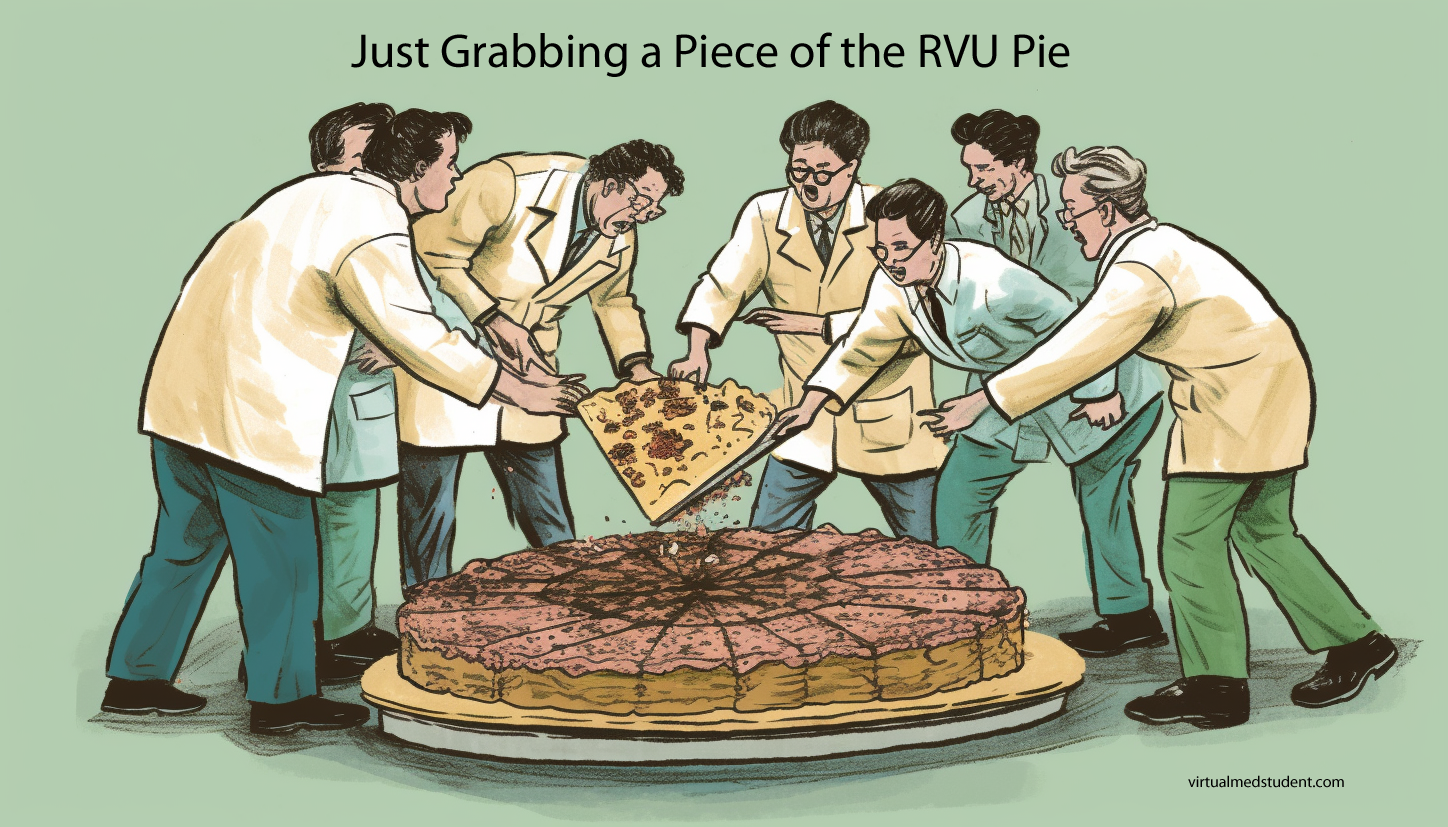
RVUs also tend to foster a lack of collegiality amongst physicians. In my experience, especially doctors on an “eat what you kill” compensation model, meaning they are paid for the number of RVUs they produce, are much less likely to refer to colleagues who may have more expertise or skill in a particular area. In other words, the doctor may “hold on” to patients to generate more RVUs rather than getting them to a colleague who may be able to provide a higher level of care for their particular ailment.
While RVUs were initially intended to standardize physician reimbursement and provide a transparent measure of physician worth, their shortcomings have become increasingly apparent over time. By focusing on quantity over quality and failing to capture the full spectrum of a physician’s value, the RVU system has inadvertently compromised patient care and perpetuated healthcare disparities. It is essential for the healthcare industry to consider alternative methods of evaluation and reimbursement that better align with the goals of patient-centered care, quality improvement, and equitable resource distribution.
It can be a fine line between incentivizing physicians to “work harder” and “earn more” while maintaining a high level of care and maintaining a highly ethical medical practice. I don’t think RVUs are a great answer to this dilemma, but for the time being it is the best we have in the United States. Let’s here your thoughts below…