Heart block, also known as atrioventricular (AV) conduction system block, refers to decreased conduction of electrical impulses through the heart. This decreased conduction occurs at the atrioventricular node of the heart’s conduction system. Heart block occurs in three flavors: type 1, type 2, and type 3. Each type has different causes and different treatments.
Pathology and Types
In type 1 AV block the PR interval on an ECG is longer than normal (> 200 msec), but every QRS complex has a preceding P-wave indicating that the electrical impulses from the atria (ie: the top chambers in the heart) are "making" it through the AV node to the ventricles. In type 1 block, the AV nodal conduction is slowed compared to normal "healthy" individuals, but the impulses are still able to get all the way through the conduction system of the heart.
Type 1 AV node block = PR interval > 200 msec, no missed beats.
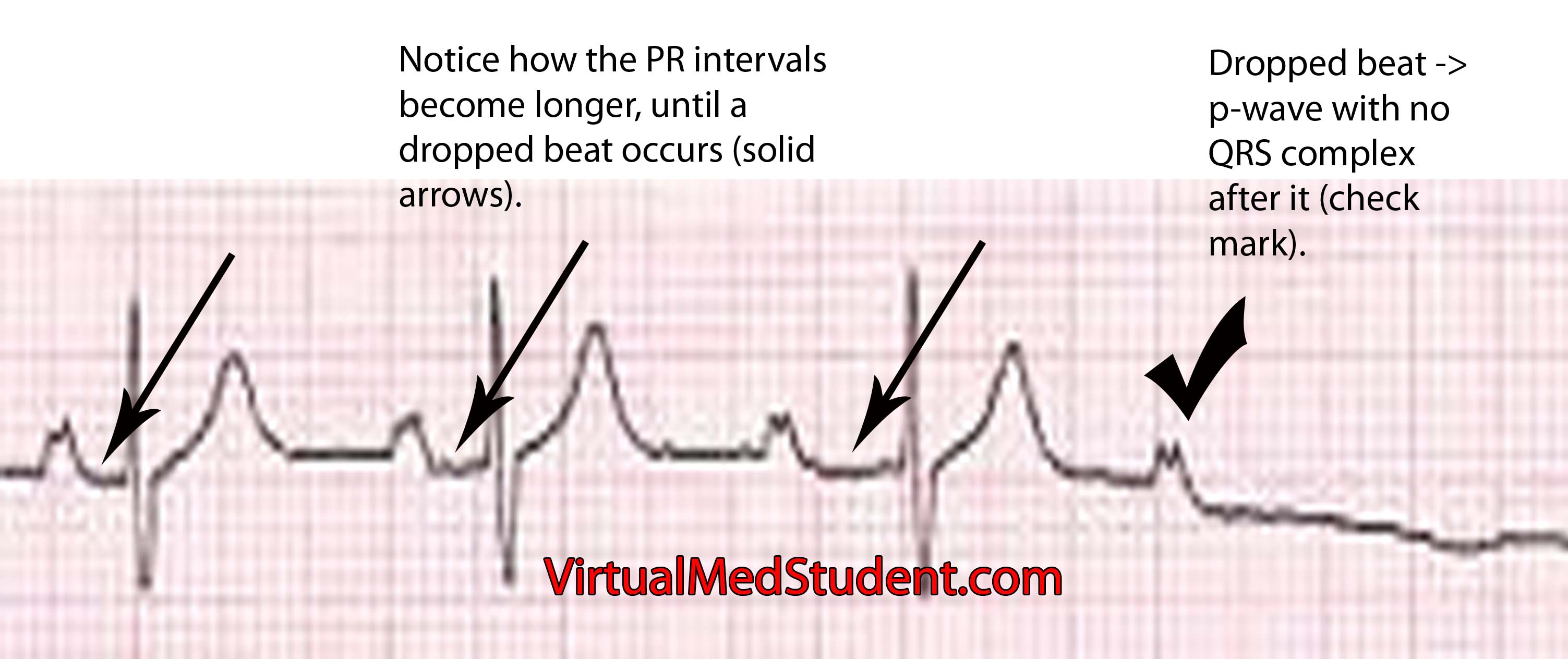
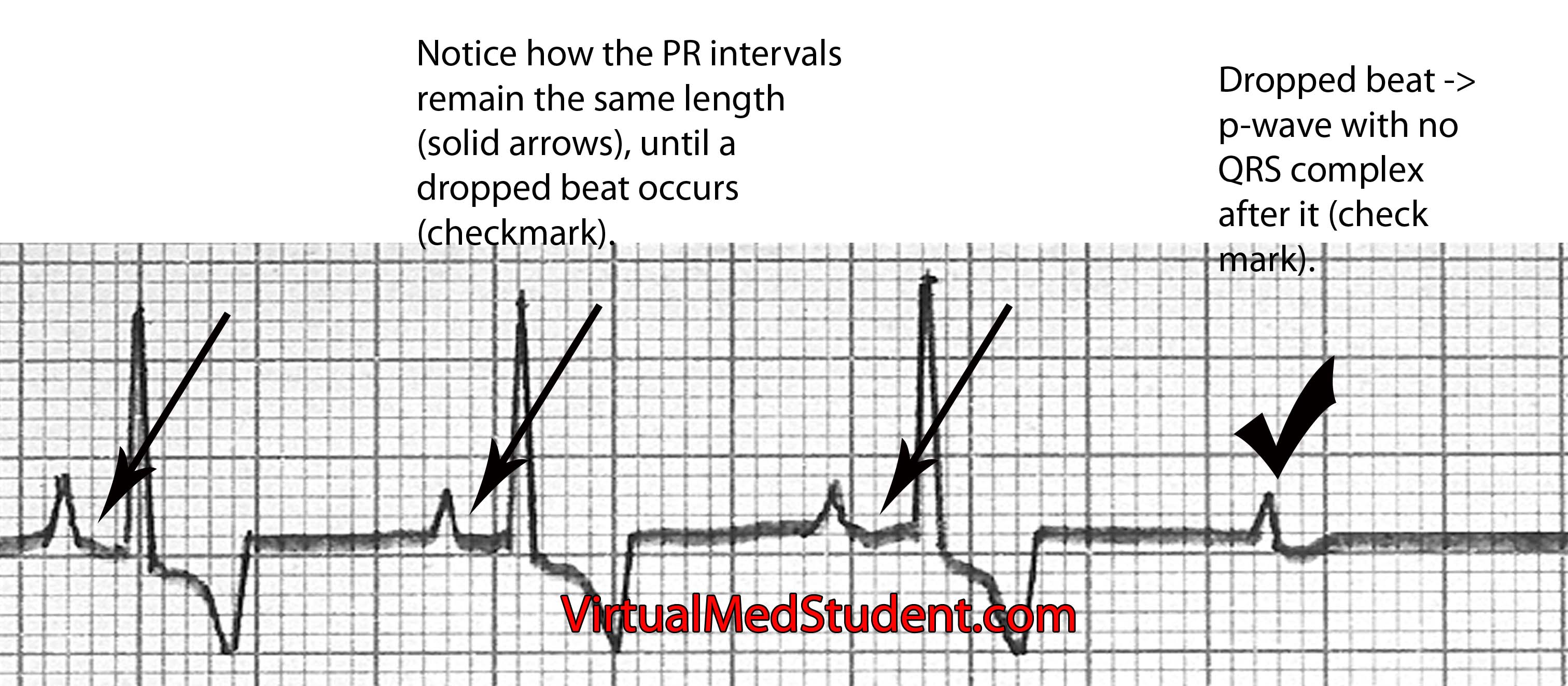
Type 2 heart block occurs in 2 flavors: Mobitz type 1 and type 2. In Mobitz type 1 the amount of delay between the P-wave and QRS complex (ie: the PR interval) gradually increases until a beat is dropped. It is caused by impaired conduction in the AV node. Mobitz type 2 occurs when the PR interval remains stable, and then out of the blue a missed beat occurs; this is caused most commonly by slowed conduction through the bundle of His or bundle branches of the heart’s conduction system.
Mobitz type 1 = increasing PR interval until dropped beat occurs (image below). Mobitz type 1 is also referred to as "Wenckeback" block.
Mobitz type 2 = PR interval remains the same until a dropped beat occurs (image below). Mobitz type 2 is also referred to as "Hay" block.
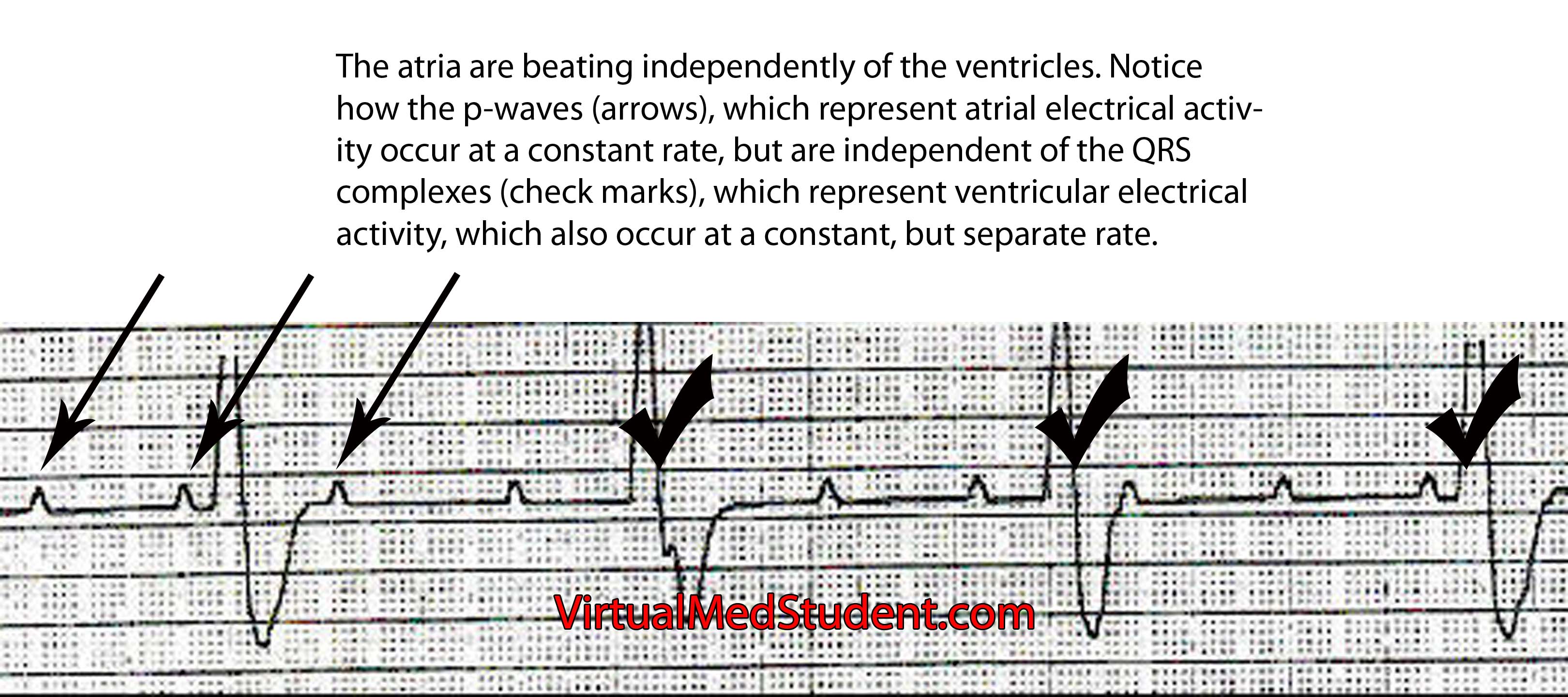
Finally, type 3 AV nodal block occurs when the atria and ventricles of the heart beat independently of one other. The most common causes of 3rd degree block are severe diseases of the AV nodal system due to age, previous heart attack, drug and medication toxicity (ie: digitalis), and untreated Lyme disease. The atria generally beat at a faster rate than the ventricles. In other words, the ECG will show more P-waves than QRS complexes. The QRS complexes may be narrow or wide depending on where in the conduction system the escape rhythm originates.
Type 3 heart block = atria (p-waves) and ventricles (QRS) beat independently of each other; no impulses from the atria make it to the ventricles (image below).
Symptoms
The symptoms of heart block depend on how slow the rate becomes. Patients with type 1 block rarely become symptomatic because the atria are still setting the pace of the entire hearts rhythm. However, in Mobitz type 2 and type 3 block the heart rate can become very slow. When this occurs symptoms such as syncope (ie: fainting), extreme fatigue, shortness of breath, and dizziness can occur. These symptoms occur because the heart is not pumping blood fast enough to keep up with the body’s demand; the result is a decrease in cardiac output.
Diagnosis
Diagnosis of heart block can be made by looking at the characteristic findings on ECG.
Treatment
Treatment of AV nodal dysfunction is dependent on the type. Most patients with type 1 heart block do not need treatment. Type 1 heart block can be considered a "healthy" variant of AV nodal conduction, which is slower than most people in the population. The only instance where type 1 block may need further work up is in elderly patients who have other signs or symptoms of coronary artery disease.
| Type | Treatment |
| Type 1 | Usually none, look for causes such as coronary artery disease in elderly patients |
Type 2 – Mobitz type 1 |
Usually none, but pacemaker if symptomatic. Also discontinue any drugs that slow AV node. |
| Type 2 – Mobitz type 2 | Pacemaker |
| Type 3 | Pacemaker |
Mobitz type 1 (ie: one of the 2 subgroups of type 2 heart block) also generally requires no treatment. If patients are symptomatic pacemaker insertion may be considered. Mobitz type 2 is more worrisome because it often progresses to 3rd degree heart block. In these patients, pacemakers are often inserted to ensure that the heart beats at a pre-defined and safe rate.
Type 3 heart block is almost always controlled with pacemaker insertion. The reason is that the ventricles often beat at a rate that is too slow for normal daily activity. A pacemaker will keep the heart beating at a pre-defined rate to ensure that symptoms do not develop.
Overview
Heart block (aka: atrioventricular block) occurs when impulses travel too slowly, or not at all through the AV node. There are different types depending on how severe the block is. In type 1 AV block impulses are slowed, but cause no conduction block. In type 2 missed beats can occur, and in type 3 the atria beat independently of the ventricles indicating complete conduction block. Symptoms depend on the severity of block but can include fainting, shortness of breath, dizziness, and fatigue. Diagnosis is made by ECG. Treatment is dependent on the type of block, but can include placement of a pacemaker.
References and Resources
- Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. Seventh Edition. Philadelphia: Elsevier Saunders, 2004.
- Lilly LS, et al. Pathophysiology of Heart Disease: A Collaborative Project of Medical Students and Faculty. Fourth Edition. Lippincott Williams and Wilkins, 2006.
- Flynn JA. Oxford American Handbook of Clinical Medicine (Oxford American Handbooks of Medicine). First Edition. Oxford University Press, 2007.