Fetal growth is most commonly monitored by ultrasound. Most “routine” pregnancies begin with one fetal ultrasound between 18 and 20 weeks of gestation. This ultrasound can pick up important defects that may not be apparent at later gestational dates. If the 18-20 week ultrasound is normal, and the pregnancy is otherwise uncomplicated, repeat ultrasounds are not routinely performed.
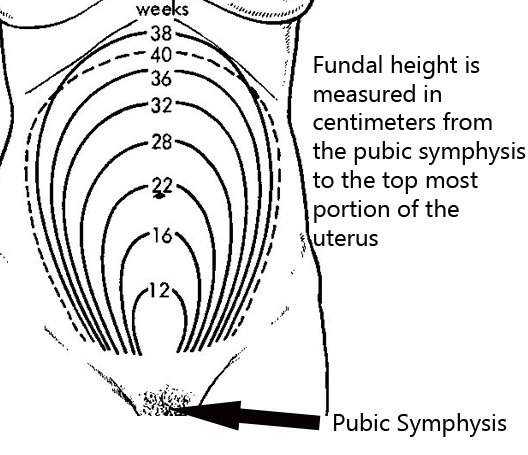
Fetal growth can also be monitored by measuring the "fundal height". The fundal height is the distance between the fundus (ie: top of the uterus), which is felt via palpation of the abdomen, and the pubic symphysis (see image to left).
A rule of the thumb is that the top of the uterus should be felt at the level of the umbilicus (ie: belly button) at approximately 20 weeks gestation. It then increases proportionally until about 36 weeks gestation. At this point the height may actually decrease as the fetal head enters the pelvis.
Fetal Maturity
There are three different ways to assess fetal maturity. They are used to determine if the fetus has adequate lung maturity to survive outside the uterus. These tests measure molecules that are present in the amniotic fluid. Therefore an invasive test known as an amniocentesis is necessary. The different methods are:
(1) Lecithin to sphingomyelin ratio
(2) Phosphatidylglycerol test
(3) Foam stability index
The first way of determining fetal lung maturity is to measure the lecithin to sphingomyelin ratio. Sphingomyelin is a specialized phospholipid that is produced in constant amounts by the fetus throughout pregnancy. Lecithin is a component of surfactant (ie: molecules that help keep the alveoli of the lung inflated) and its production increases as fetal lung maturity increases. An L:S ratio of greater than two indicates that the fetal lungs are mature enough to work outside the uterus.
The second test is known as the phosphatidylglycerol (PG) test. The presence of this molecule in the amniotic fluid indicates fetal lung maturity. PG is a component of pulmonary surfactant, which helps keep the gas exchange portions of the lung (ie: alveoli) from deflating at the end of exhalation.
The third test is the "foam stability index" test. This test measures the stability of bubbles when amniotic fluid is shaken with variable percent alcohol solutions. If the bubbles are stable this indicates fetal lung maturity.
Fetal Well-Being
Fetal well-being is assessed using several different methods. They include:
(1) Non-stress test
(2) Stress test
(3) Biophysical profile
Then on-stress test measures fetal well-being by looking at changes in the fetal heart rate during movement. A normal (aka: "reactive") non-stress test occurs when the fetus’ heart rate increases by 15 beats per minute over 15 seconds following fetal movement. If this increase in heart rate occurs twice within 20 minutes of monitoring the test is normal or “reactive”. Note: if the fetus is less than 32 weeks gestation then only a 10 beat per minute increase is needed to satisfy the non-stress test.
The stress test (aka: "contraction stress test", or "oxytocin stress test" depending on how contractions are elicited) measures the fetus’ ability to handle the "stress" of a uterine contraction. When the uterus contracts blood flow from the placenta is momentarily decreased. A healthy fetus will have no discernible change in their heart rate; however, an at risk fetus will have heart rate decelerations. Stress tests, especially oxytocin induced stress tests, commonly result in false-positives (ie: indicate fetal jeopardy when the fetus is normal); therefore, an abnormal stress test is followed by a non-stress test. If the non-stress test is normal/reactive then the stress test is often times considered a false-positive.
The biophysical profile uses five parameters for assessing fetal well-being. They include: fetal breathing movements, gross body movements, fetal muscle tone, fetal heart rate as measured by non-stress test, and qualitative amniotic fluid levels. Each of these parameters is given a score of 0 if absent/abnormal, or 2 if normal. A score of 8-10 is reassuring and indicates no problems with the fetus.
Related Articles
References and Resources
- Wagner B, Meirowitz N, Shah J, et al. Comprehensive Perinatal Safety Initiative to Reduce Adverse Obstetric Events. J Healthc Qual. 2011 Mar 1.
- Whitworth M, Bricker L, Neilson JP, et al. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2010 Apr 14;(4):CD007058.
- Beckmann CRB, Ling FW, Smith RP, et al. Obstetrics and Gynecology
. Fifth Edition. Philadelphia: Lippincott Williams and Wilkins, 2006.
- Bickley LS, Szilagyi PG. Bates’ Guide to Physical Examination and History Taking
. Ninth Edition. New York: Lippincott Williams and Wilkins, 2007.