Medulloblastomas are highly malignant brain tumors. They are the most common primary malignant brain tumor, and the second most common overall brain tumor in children. They are uncommonly seen in adults. Medulloblastomas are believed to arise from the granular cell layer of the cerebellum and are part of a broader category of tumors known as primitive neuroectodermal tumors (PNETs, coolloquially called "peanuts").
The term medulloblastoma is somewhat of a misnomer because it actually comprises several distinct pathologic types. These types include classic medulloblastoma, desmoplastic/nodular medulloblastoma, large cell medulloblastoma, anaplastic medulloblastoma, and medulloblastoma with extensive nodularity.
In addition to their pathologic appearance, medulloblastomas vary in their molecular make-up. There are currently four molecular categories. They include those that belong to the sonic hedgehog gene group (SHH), the wingless gene group (WNT), and two less well understood groups known as "group three" and "group four".
The SHH group contains roughly a third of all medulloblastomas. Aberrant activation of the SHH gene is responsible for the development of all pathologic types of medulloblastomas, but is most commonly seen in anaplastic, desmoplastic, and large cell types.
The least common molecular group is the WNT group. The wingless gene signaling pathway is extremely complicated and outside the scope of this article. Suffice it to say that aberrant activation of the WNT gene can cause medulloblastoma formation, most commonly of the classic variety.
The molecular nature of group three and four is still poorly understood.
As you can see, the classification of medulloblastomas is quite complex! Medulloblastomas can be categorized both molecularly and pathologically. The table below attempts to organize the complex nature of this heterogeneous group of tumors:
| Pathologic Type | Molecular Type | Clinical Features | Outcome |
| Classic | SHH, WNT, group 3 and group 4 | Midline location, mostly in children < 10 years old, second peak in 20 to 40 year olds | Better prognosis |
| Large cell | Group 3, group 4, SHH | Uncommon, similar to anaplastic | Worse prognosis |
| Anaplastic | Group 3, group 4, SHH | Midline with cysts, necrosis, and bleeding within tumor | Worse prognosis |
| Desmoplastic | SHH | Located in the midline in children and off midline in adults | Better prognosis |
| Extensive nodularity | SHH | Off midline and nodular architecture | Better prognosis |
Given the malignant nature of these tumors it is not uncommon for medulloblastomas to seed other areas of the central nervous system. Tumor frequently "coats" the spinal cord. These lesions are known as "drop" metastasis and are seen in 10% to 40% of patients at the time of diagnosis.
Signs and Symptoms
Patients with medulloblastoma can present with a variety of signs and symptoms. Headaches with nausea and vomiting secondary to obstructive hydrocephalus is frequently observed. In addition, signs of brainstem dysfunction including dizziness and trouble with eye movements may occur. Cerebellar signs like ataxia and dysdiadochokinesia are also commonly seen.
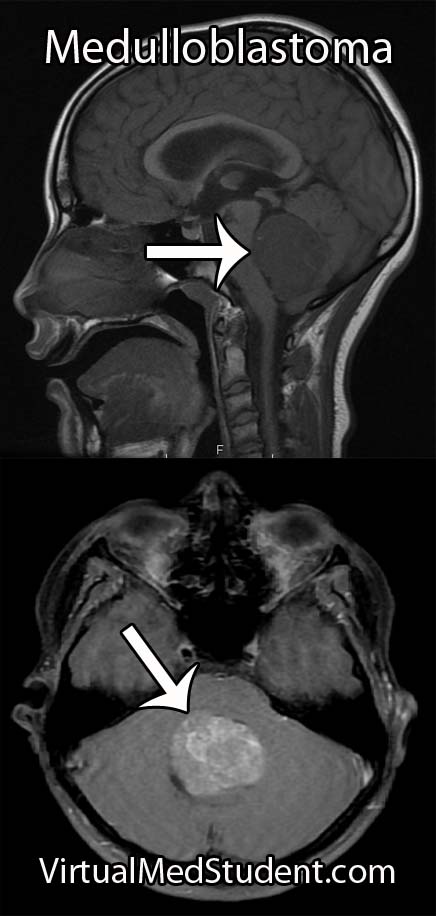
Diagnosis
Treatment
Treatment is composed of surgical removal of the tumor, chemotherapy, and radiation. Surgery is always the first treatment because it decreases the disease "burden" so that radiation and chemotherapy can effectively treat any remaining tumor cells.
After surgery patients are classified as either “standard risk patients” or “poor risk patients”. Standard risk patients have complete surgical removal of their tumors and no dissemination of the disease to other areas of the central nervous system (ie: no “drop mets”). Poor risk patients have more than 1.5 cm2 of tumor left after surgery and evidence of dissemination in the cerebrospinal fluid.
Numerous chemotherapeutic medications including carboplatin, etoposide, cisplatin, cyclophosphamide, and vincristine have helped improve survival in poor risk patients. In addition, radiation therapy to the entire cranio-spinal axis has been shown to reduce recurrence rates.
Overview
Medulloblastoma is considered a malignant primitive neuroectodermal tumor. They are the second most common brain tumor in children, and the most common malignant brain tumor in children. They are rare in adults. There are several pathologic and molecular "sub-categories" of medulloblastoma; each category has different clinical features and outcome. Diagnosis is made with characteristic imaging findings in conjunction with pathologic analysis made at time of surgical resection. Treatment consists of surgery, radiation, and chemotherapy.
Related Articles
References and Resources
- Northcott PA, Hielscher T, Dubuc A, et al. Pediatric and adult sonic hedgehog medulloblastomas are clinically and molecularly distinct. Acta Neuropathol. 2011 Aug;122(2):231-40.
- Jones DT, Jäger N, Kool M, et al. Dissecting the genomic complexity underlying medulloblastoma. Nature. 2012 Aug 2;488(7409):100-5.
- Northcott PA, Jones DT, Kool M, et al. Medulloblastomics: the end of the beginning. Nat Rev Cancer. 2012 Dec;12(12):818-34.
- Byrd T, Grossman RG, Ahmed N. Medulloblastoma-biology and microenvironment: a review. Pediatr Hematol Oncol. 2012 Sep;29(6):495-506.
- Robertson PL, Muraszko KM, Holmes EJ, et al. Incidence and severity of postoperative cerebellar mutism syndrome in children with medulloblastoma: a prospective study by the Children’s Oncology Group. J Neurosurg. 2006 Dec;105(6 Suppl):444-51.
- Allen J, Donahue B, Mehta M, et al. A phase II study of preradiotherapy chemotherapy followed by hyperfractionated radiotherapy for newly diagnosed high-risk medulloblastoma/primitive neuroectodermal tumor: a report from the Children’s Oncology Group (CCG 9931). Int J Radiat Oncol Biol Phys. 2009 Jul 15;74(4):1006-11.
- Packer RJ, Gajjar A, Vezina G, et al. Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol. 2006 Sep 1;24(25):4202-8.