The axis, or second cervical vertebrae (C2), is unique amongst the vertebrae of the spine. It contains a body, which has an elongated structure that extends towards the head known as the dens (aka: odontoid). It also contains a ring-like structure that extends around the spinal cord, which is composed of the pedicles, pars interarticularis, and lamina. It forms joints with the atlas (ie: first cervical vertebrae) above it, and the third cervical vertebrae below it. It also has two foramen transversarium on either side, which are conduits for the vertebral arteries.
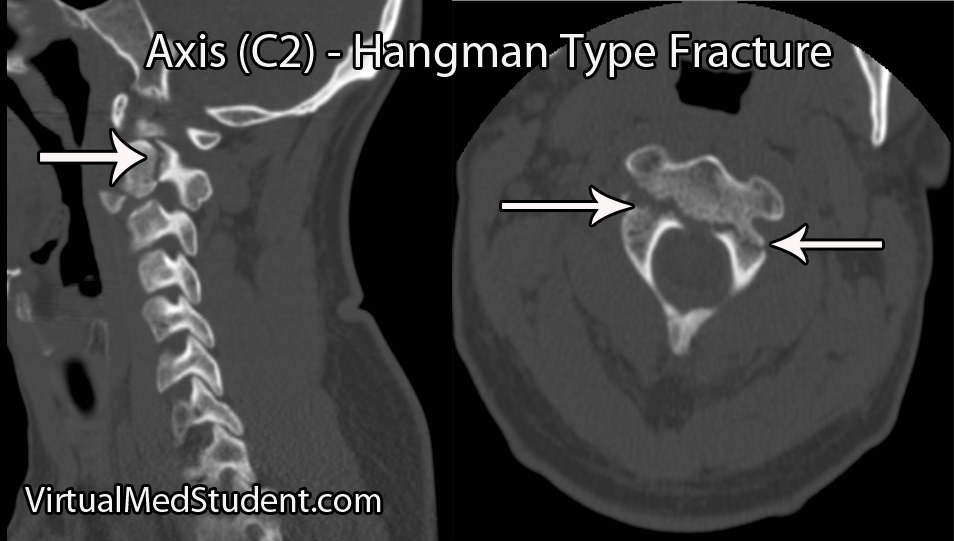
A hangman’s fracture is a break in both pedicles and/or pars interarticulari. The terms pedicle and pars interarticularis are not as well defined at C2 as they are for the other vertebrae, and thus have to be more clearly delineated before we discuss the details of a hangman’s fracture.
The pars interarticulari of C2 are the narrow pieces of bone that sit between the superior articulating facets (ie: the portion of bone that allows C2 to form a joint with C1) and the inferior articulating facets (ie: the portion of bone that allows C2 to form a joint with C3) of C2. The pedicles lie more anterior and are defined as the bony "bridges" that lie underneath the superior articulating facet and just medial (ie: closer to the spinal cord) to the transverse foramen, which house the vertebral arteries.
So now let’s get to the good stuff… Why do these fractures happen? Extension of the neck! This is why they are colloquially termed "Hangman’s" fractures; in the old days when a person was hanged the noose would pull the mandible upwards and cause the neck to violently extend. The end result was a tremendous amount of force on the pars interarticulari and pedicles of C2 leading to a fracture.
Since hangings are infrequent in today’s society, a more common cause of hyperextension of the neck is a head hitting the steering wheel or windshield of a car.
The hyperextension also often causes significant anterior ligamentous injury. The anterior longitudinal ligament (ie: the ligament that runs down the front of the spine) and the annulus fibrosis of the C2 disc are often ruptured. These findings are consistent with a hyperextension injury as the ligaments in the front get stretched to the point of rupture.
Signs and Symptoms
Surprisingly, hangman’s fractures rarely cause neurological injury. Most patients are neurologically intact meaning that there is no injury to the spinal cord and/or nerves at the level of the fracture. Typically there is neck pain, which is the most common symptom.
It is important to realize that many patients with hangman’s fractures will also have co-existent head trauma, and roughly a third of patients will have additional spine fractures. So keep a look out for associated injuries!!!
Diagnosis
The diagnosis of a hangman’s fracture can be made using x-rays and CT scans. MRI scans are also frequently ordered to determine the extent of co-existent ligamentous and soft tissue injury. A CT angiogram or MR angiogram should also be done to assess for co-existent vertebral artery injury.
There are several different grading systems for hangman’s fractures. They include the Effendi, Francis, and Levine and Edwards classifications.
The Effendi system is based on the orientation of the fracture, as well as the degree of angulation and dislocation between C2 on C3.
The Francis system also takes into account the angulation and displacement between the bodies of C2 and C3, which is measured between the inferior endplate of C2 and the superior endplate of C3.
Perhaps the easiest to implement clinically is the Levine and Edwards classification. A type I Levine fracture is a non-displaced, non-angulated fracture. Type II fractures come in two flavors: type II is a fracture that is significantly angulated (ie: > 11 degrees) and displaced (ie: greater than 3mm) and a type IIa fracture is angulated (ie: greater than 11 degrees), but not significantly displaced. Type III fractures are fracture-dislocations of C2 on C3.
The Levine and Edwards’ Classification System |
|||
| Type | Angulation | Displacement | Treatment |
| Type I | Minimal | Minimal | Rigid orthotic |
| Type II | Greater than 11 degrees | Greater than 3mm | Traction ± rigid orthotic ± surgery |
| Type IIa | Greater than 11 degrees | Minimal | Traction ± rigid orthotic ± surgery |
| Type III | Minimal to severe | Significant (fracture/dislocation) | Traction + surgery |
Treatment
Most isolated hangman’s fractures can be treated with external immobilization in a rigid cervical collar (ie: Miami J or Philadelphia collar) or in a halo immobilization device.
However, if there is significant ligamentous disruption, severe angulation and/or dislocation, or the inability to obtain adequate alignment of the spine in an immobilization device (ie: rigid collar or halo) then internal surgical fixation and fusion should be performed.
The need for surgery depends on the severity of the fracture and/or the integrity of the associated ligaments and discs.
A surgical approach from the front (aka: an "anterior" approach) may be performed to fuse the C2 and C3 vertebrae by removing the disc material between them. This approach is most often done in the presence of anterior longitudinal ligament rupture and/or intervertebral disc protrusion (ie: a "traumatic" disc).
Surgery from behind may also be used (aka: a "posterior" approach). Usually, the 1st through 3rd cervical vertebrae are incorporated into the fusion process, but some surgeons may opt to fuse to the base of the skull in cases of more severe injuries.
Overview
Hangman’s fractures occur after violent extension of the neck. The pedicles or pars interarticulari are fractured on both sides of the C2 ring. Neurological injury is rare in isolated hangman’s fractures, but frequently there are associated injuries to other bones in the cervical spine, as well as injuries to the brain and face. Diagnosis is made with x-rays, CT scans, and MRI. Treatment is with rigid immobilization of the cervical spine and/or surgical fixation depending on the extent of injury.
Related Articles
- Os odontoideum
- Dislocated cervical facet
- Spondylolysis
- Odontoid (C2) fractures
- Thoracolumbar burst fractures
- Atlas (C1) fractures
References and Resources
- Ebraheim NA, Fow J, Xu R, et al. The location of the pedicle and pars interarticularis in the axis. Spine (Phila Pa 1976). 2001 Feb 15;26(4):E34-7.
- White AA, Panjabi MM. Clinical Biomechanics of the Spine
. Philadelphia: Lippincott, 1990.
- Effendi B, Roy D, Cornish B, et al. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63-B(3):319-27.
- Fielding JW, Francis WR Jr, Hawkins RJ, et al. Traumatic spondylolisthesis of the axis. Clin Orthop Relat Res. 1989 Feb;(239):47-52.
- Greenberg MS. Handbook of Neurosurgery
. Sixth Edition. New York: Thieme, 2006. Chapter 25.
- Yanni DS, Perin NI. Fixation of the axis. Neurosurgery. 2010 Mar;66(3 Suppl):147-52.
- Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985 Feb;67(2):217-26.