Multiple sclerosis literally means “multiple scars”. And in multiple sclerosis the scaring takes place in the central nervous system. The pathology of why multiple sclerosis occurs is not yet fully understood. We do know that it is an autoimmune condition in which the body attacks itself.
The target of that attack is myelin. Myelin is a fatty substance that insulates neuronal axons. You can think of myelin as the rubber coating around electrical wiring. The insulating role of myelin helps axons send information rapidly from one neuron to the next. Interestingly, multiple sclerosis only affects myelin created by oligodendrocytes, which are glial cells (ie: neuron support cells) found in the central nervous system. Multiple sclerosis does not affect myelin formed by Schwann cells, which are located in the peripheral nervous system.
The damage to myelin is thought to be caused by T-cells. T-cells are a branch of the adaptive immune system. T-cells do not normally invade the central nervous system, but in multiple sclerosis some antecedent event (possibly infection?) allows T-cells to gain access to the CNS. In genetically susceptible people these trapped T-cells "see" myelin as a foreign substance and attack it. The result is inflammation and scaring (in the brain, scaring is called "gliosis").
Signs and Symptoms
Although multiple sclerosis can occur in all races and in both genders, it tends to affect women of European descent more frequently. In addition, patients who live at higher latitudes also seem to be at higher risk.
The classic presentation of someone with multiple sclerosis is numerous neurological complaints spaced out in time. These neurological symptoms can be highly variable. Often times patients will have blurred vision or blindness if demyelination occurs at the optic nerve. This is known as optic neuritis and is a common feature in multiple sclerosis patients.
In addition, weakness of an extremity can occur and can be partial (paresis) or complete (paralysis). Difficulty speaking and swallowing can occur, as can bowel and bladder incontinence. Sensory deficits like numbness and tingling are also common. If the cerebellum or spinocerebellar tracts in the spinal cord are involved loss of coordination can occur (ataxia).
There are many other symptoms that can be seen in multiple sclerosis depending on which part of the central nervous system is involved. Ultimately, if a patient returns with several neurological complaints spaced out in time, then multiple sclerosis should be on the list of possible diagnoses.
Diagnosis
The diagnosis of multiple sclerosis is based on clinical and supporting laboratory evidence. There is no single test that can determine if it is present, but there is a set of guidelines that can help the clinician make the diagnosis, which include:
(1) Signs and symptoms referable to the central nervous system.
(a) Symptomatic episodes should last at least 24 hours.
(b) Two or more symptomatic episodes at least one month apart.
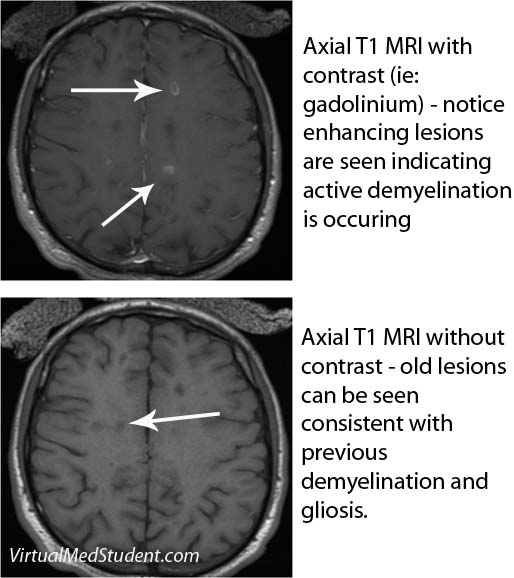
(2) Two or more lesions (ie: “scars”) seen on MRI of the brain (see image below).
(3) Physical exam findings supporting central nervous system disease.
(4) Cerebrospinal fluid results consistent with a diagnosis of multiple sclerosis.
(5) No other disease(s) that could explain the symptoms and findings.
Many other tests are often performed to rule out other causes for the patient’s symptoms. Testing for systemic lupus erythematosis, Lyme disease, neuro-syphilis, vitamin B12 deficiency, and thyroid disease are common adjunctive tests.
Treatment
There is currently no cure for multiple sclerosis. However, like many other autoimmune disorders, there are several disease modifying medications that can slow its progression.
The first class of modifying medications are known as the "interferons". Interferon is believed to act through several different mechanisms. It inhibits white blood cell proliferation (T-cells are one type of white blood cell) and decreases antigen presentation by immune cells. It also reduces T-cell migration and switches the body towards an anti-inflammatory state. These effects help decrease the inflammation associated with multiple sclerosis. There are currently three different formulations of interferon on the market for multiple sclerosis. The first two are interferon β-1a formulations known as Avonex® and Rebif®. The third is an interferon β-1b formulation known as Betaseron®.
Another medication known as glatiramer acetate (aka: Copaxone®) acts as a possible myelin "mimick", protecting normal myelin from attack. Glatiramer is a synthetic polymer of four amino acids (ie: the building blocks of protein) found in normal human myelin. The exact mechanism of glatiramer’s actions are unknown.
Natalizumab (aka: Tysabri®) is approved for use in multiple sclerosis. It is a monoclonal antibody that binds to, and inhibits, the function of α4-integrin. α4-integrin is a cell adhesion molecule found on white blood cells that normally allows them to move into body tissues to fight infection. By blocking this movement, natalizumab is thought to decrease the number of T-cells that enter the central nervous system.
Another medication known as mitoxantrone is also used in the treatment of multiple sclerosis. It was originally designed as a cancer medication. Its mechanism of action is to disrupt DNA synthesis and repair by inhibiting a protein known as topoisomerase.
Patients who are acutely symptomatic (ie: having a "flair") are treated with intravenous steroids. Methylprednisolone is the most common steroid used in patients with acute neurological symptoms.
The goal of all of these medications is to dampen the immune response and prevent the abnormal inflammation that occurs in multiple sclerosis. Because of this, many of these medications have side effects such as the risk of infections.
Finally, depending on a patient’s symptoms, therapies designed to mitigate them may be used as well. Medications like baclofen are commonly used for spasticity; dalfampridine (Ampyra®) can help patients walk longer distances. It is important to prescribe medications that can palliate some of the symptoms.
Overview
Multiple sclerosis is an autoimmune condition in which the body attacks the myelin surrounding axons in the central nervous system (ie: the “insulation around the wires”). Symptoms are numerous and depend on what area of the brain and/or spinal cord is being “attacked”. Everything from weakness to blindness can occur. Diagnosis is based on clinical signs and symptoms, as well as supporting evidence such as MRI findings and cerebrospinal fluid abnormalities. Treatment is with various disease modifying agents as well as medications designed to treat symptoms from MS.
Related Articles
References and Resources
- Baehr M, Frotscher M. Duus’ Topical Diagnosis in Neurology: Anatomy, Physiology, Signs, Symptoms
. Fourth Edition. Stuttgart: Thieme, 2005.
- Simon RP, Aminoff MJ, Greenberg DA. Clinical Neurology, Seventh Edition (LANGE Clinical Medicine)
. Seventh Edition. New York: McGraw Hill, 2009.
- Flynn JA. Oxford American Handbook of Clinical Medicine (Oxford American Handbooks of Medicine)
. First Edition. Oxford University Press, 2007.
- Dutta R, Trapp BD. Mechanisms of neuronal dysfunction and degeneration in multiple sclerosis. Prog Neurobiol. 2010 Oct 12. [Epub ahead of print] Dutta R, Trapp BD.