Tuberculosis is one of the most common infectious diseases in the world. It is caused by a bacteria of the genus mycobacterium. Tuberculosis usually infects the lungs, but may also infect the lymph nodes, vertebral bodies, kidneys, gastrointestinal system, or central nervous system.
Central nervous system disease comes in two flavors: a focal abscess-like lesion known as a tuberculoma or tuberculosis meningitis. The remainder of this article will focus on tuberculosis meningitis, which is an uncommon (although not rare!) form of extra-pulmonary tuberculosis.
Let’s start by discussing how the bacteria get into the central nervous system. After being inhaled the bacteria infect cells known as macrophages. The infected macrophages move towards lymph nodes, and eventually end up in the blood stream. Once in the blood stream, the mycobacterium-infected macrophages can travel anywhere in the body!
One spot the bacterium hitch a ride to is the lining of the brain (aka: the meninges). Collections of mycobacterium-laden macrophages (“Rich foci”) can rupture into the subarachnoid space causing an inflammatory reaction (ie: a "meningitis", or inflammation of the meninges).
For unclear reasons, the inflammation seen in tuberculosis meningitis preferentially affects the basal cisterns and base of the brain. Autopsy specimens show a gelatinous material coating the undersurface of the brain. The inflammatory reaction is what causes the signs and symptoms of tuberculosis meningitis.
Signs and Symptoms
Tuberculosis meningitis can present in a number of different ways. Many patients present with days to months of non-specific symptoms such as headache, lethargy, nausea, and vomiting.
Cranial neuropathies are commonly seen, especially since tuberculosis meningitis affects the basal cisterns and base of the brain, which is where many of the cranial nerves run.
Additionally, up to 40% of patients may present with stroke. Strokes occur because the inflammation can "eat up" the linings of small blood vessels. The basal ganglia, internal capsule, and thalamus are the most common locations where strokes occur in tuberculosis meningitis.
Diagnosis
The clinical history is extremely important. Tuberculosis meningitis may affect both immunocompetent and immunocompromised (ie: think HIV/AIDs, diabetics, people on immunosuppressives, etc.) people. If the clinical history and physical exam findings are concerning for meningitis, than confirmatory studies should be performed.
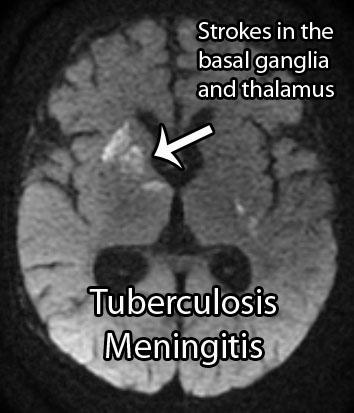
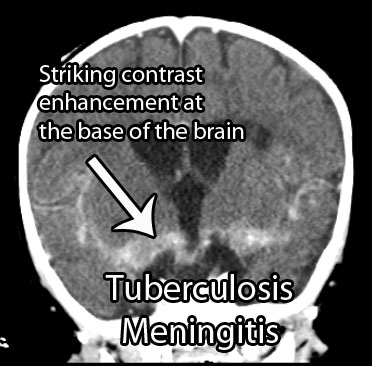
Appropriate imaging studies include CT or MRI scans with contrast. The basal cisterns and base of the brain will "light up" with contrast because of inflammation. Imaging may also show strokes and hydrocephalus. Under the right clinical scenario imaging studies can help support the diagnosis, but are not specific.
Treatment
Treatment should consist of antibiotics that target mycobacterium tuberculosis. Commonly used antibiotics include rifampin, isoniazid, streptomycin, and pyrazinamide. Other antibiotics may be necessary if the strain of bacteria is resistant to these drugs.
Steroids are also frequently given to help reduce inflammation. Dexamethasone, a commonly used steroid, has been shown to improve survival rates (although it may not affect outcome in those that survive).
The intense inflammatory reaction seen in tuberculosis meningitis may gunk up the re-absorption of cerebrospinal fluid and cause a communicating hydrocephalus. Hydrocephalus occurs in 70% of cases and may require surgically inserted shunts to fix.
Overview
Tuberculosis meningitis is a devastating manifestation of a common infectious disease. It can cause cranial neuropathies, strokes, and hydrocephalus. Prompt diagnosis is mandatory and is made from the clinical history, CSF analysis, and imaging studies. Treatment is with anti-TB medications and steroids. Many survivors have long term disabilities despite appropriate treatment.
Related Articles
References and Resources
- Thwaites GE, Nguyen DB, Nguyen HD, et al. Dexamethasone for the treatment of tuberculous meningitis in adolescents and adults. N Engl J Med. 2004 Oct 21;351(17):1741-51.
- Chin JH, Mateen FJ. Central Nervous System Tuberculosis: Challenges and Advances in Diagnosis and Treatment. Curr Infect Dis Rep. 2013 Oct 12.
- Woldeamanuel YW, Girma B. A 43-year systematic review and meta-analysis: case-fatality and risk of death among adults with tuberculous meningitis in Africa. J Neurol. 2013 Aug 21.
- van der Harst JJ, Luijckx GJ. Treatment of central nervous system tuberculosis infections and neurological complications of tuberculosis treatment. Curr Pharm Des. 2011;17(27):2940-7.