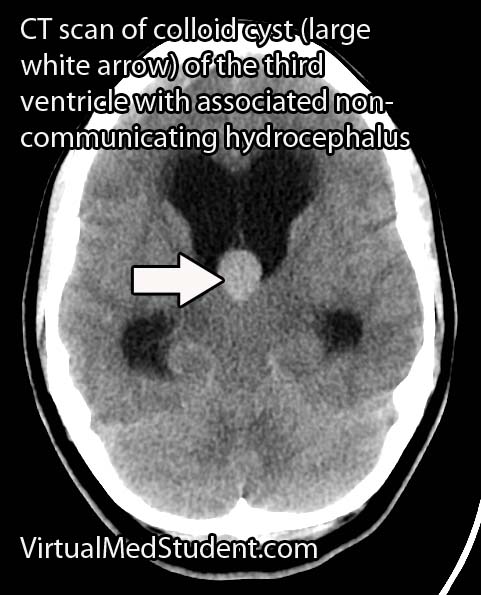
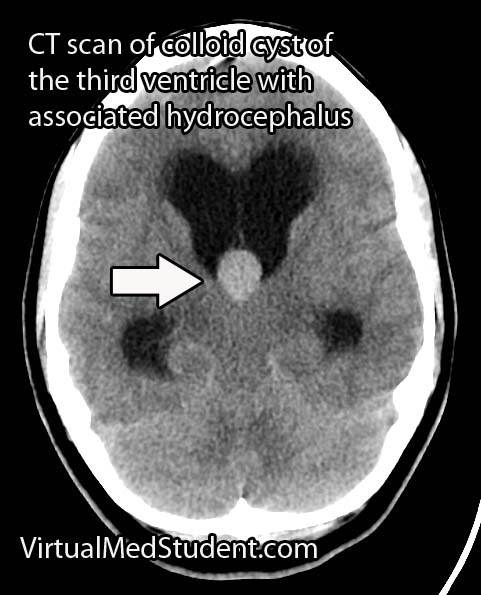
Colloid cysts of the third ventricle are slow-growing, benign cranial tumors. They are believed to be composed of an epithelial wall with either mucous or protein like material trapped inside a spherical structure. However, their exact etiology is still under debate.
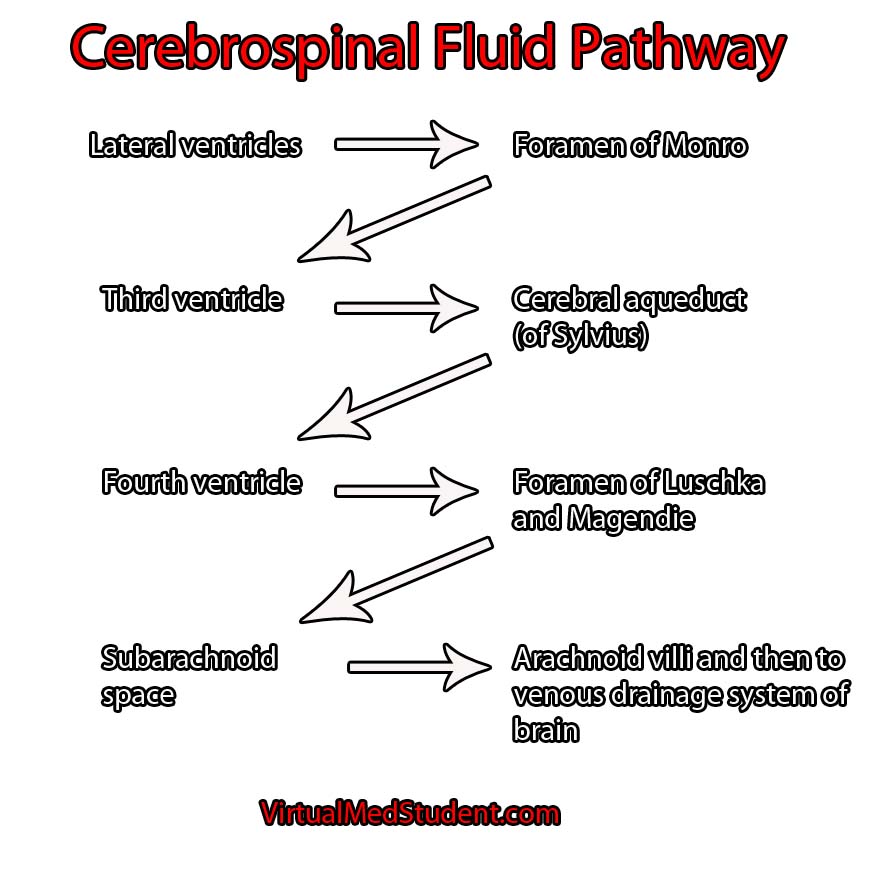
They are typically found in the anterior portion of the third ventricle near the foramen of Monroe (the channels that connect the lateral ventricles to the third ventricle). The third ventricle is one of the spinal fluid filled cavities of the brain.
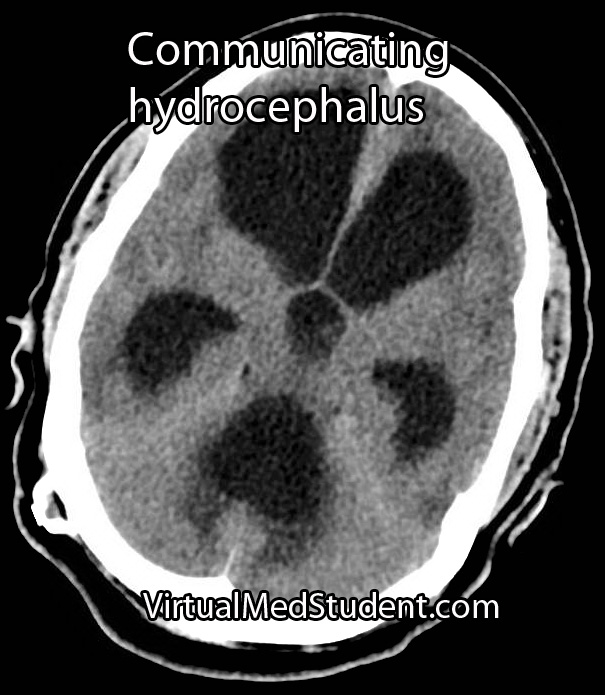
Colloid cysts are “benign” because they are not cancerous (ie: don’t invade other parts of the body); however, they have the potential to block the flow of cerebrospinal fluid, which can lead to acute hydrocephalus and brain herniation. Therefore, in this regards they are certainly not “benign” tumors!
Signs and Symptoms
The most common presenting symptom of a colloid cyst is headache and difficulty walking. Acute hydrocephalus (dilation of the ventricular system secondary to blocked cerebrospinal fluid) can occur if the cyst blocks the flow of cerebrospinal fluid; this can cause nausea, vomiting, headache, and lethargy. Changes in mental status may also be seen in patients with these lesions.
There are numerous reports of patients dying suddenly from colloid cysts of the third ventricle. This is believed to be due to rapid obstruction of cerebrospinal fluid at the foramen of Monroe. The fluid builds up behind the blockage which puts pressure on the brain. Too much pressure can cause the brain to herniate through the base of the skull (see the Monro-Kellie doctrine).
Diagnosis

Treatment
Treatment of colloid cysts is surgical. There are numerous approaches including the use of an endoscope, or the use of stereotactic guidance systems. In patients with contraindications to surgery bilateral cerebrospinal fluid shunts can be placed to prevent acute hydrocephalus from developing.
Overview
Colloid cysts of the third ventricle are "benign" tumors. They have the potential to block the flow of cerebrospinal fluid leading to acute hydrocephalus. The most common symptom is headache followed by gait instability. Diagnosis is made with CT and MRI imaging. Treatment is surgical resection.
Related Articles
References and Resources
- Boogaarts HD, Decq P, Grotenhuis JA, et al. Long-term results of the neuroendoscopic management of colloid cysts of the third ventricle: a series of 90 cases.Neurosurgery. 2011 Jan;68(1):179-87.
- Nagaraju S, O’Donovan DG, Cross J, et al. Colloid cyst of the third cerebral ventricle with an embryological remnant consistent with paraphysis cerebri in an adult human. Clin Neuropathol. 2010 May-Jun;29(3):121-6.
- Greenberg MS. Handbook of Neurosurgery
. Sixth Edition. New York: Thieme, 2006. Chapter 25.
- Kondziolka D, Bilbao JM. An immunohistochemical study of neuroepithelial (colloid) cysts. J Neurosurg. 1989 Jul;71(1):91-7.
- Stachura K, Libionka W, Moskala M, et al. Colloid cysts of the third ventricle. Endoscopic and open microsurgical management. Neurol Neurochir Pol. 2009 May-Jun;43(3):251-7.