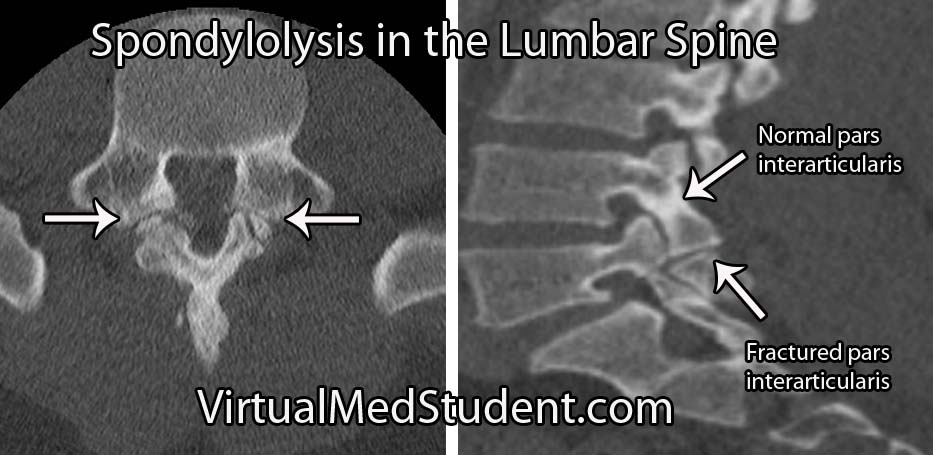
The CT scan below shows the relevant anatomy of a normal pars interarticularis and one that exhibits spondylolysis. Spondylolysis occurs about 85% of the time at the fifth (L5) lumbar segment, followed in frequency by the fourth lumbar vertebrae (L4), but it can occur elsewhere in the spine.
In spondylolysis there is a fracture/defect in the pars. Fractures of the pars interarticularis typically occur after repeated extension of the lower back. Repetitive extension causes significant pressure on the pars, which in susceptible individuals can lead to weakening of the bone.
Spondylolysis is actually quite common in gymnasts, football, and tennis players because of the repetitive back extension required of these athletes.
The importance of spondylolysis is not so much the pars defect itself, but the fact that these defects can cause one vertebrae to "slip" over the top of the one below it. When this occurs a new name is given to the condition – spondylolisthesis.
Signs and Symptoms
Diagnosing Spondylolysis
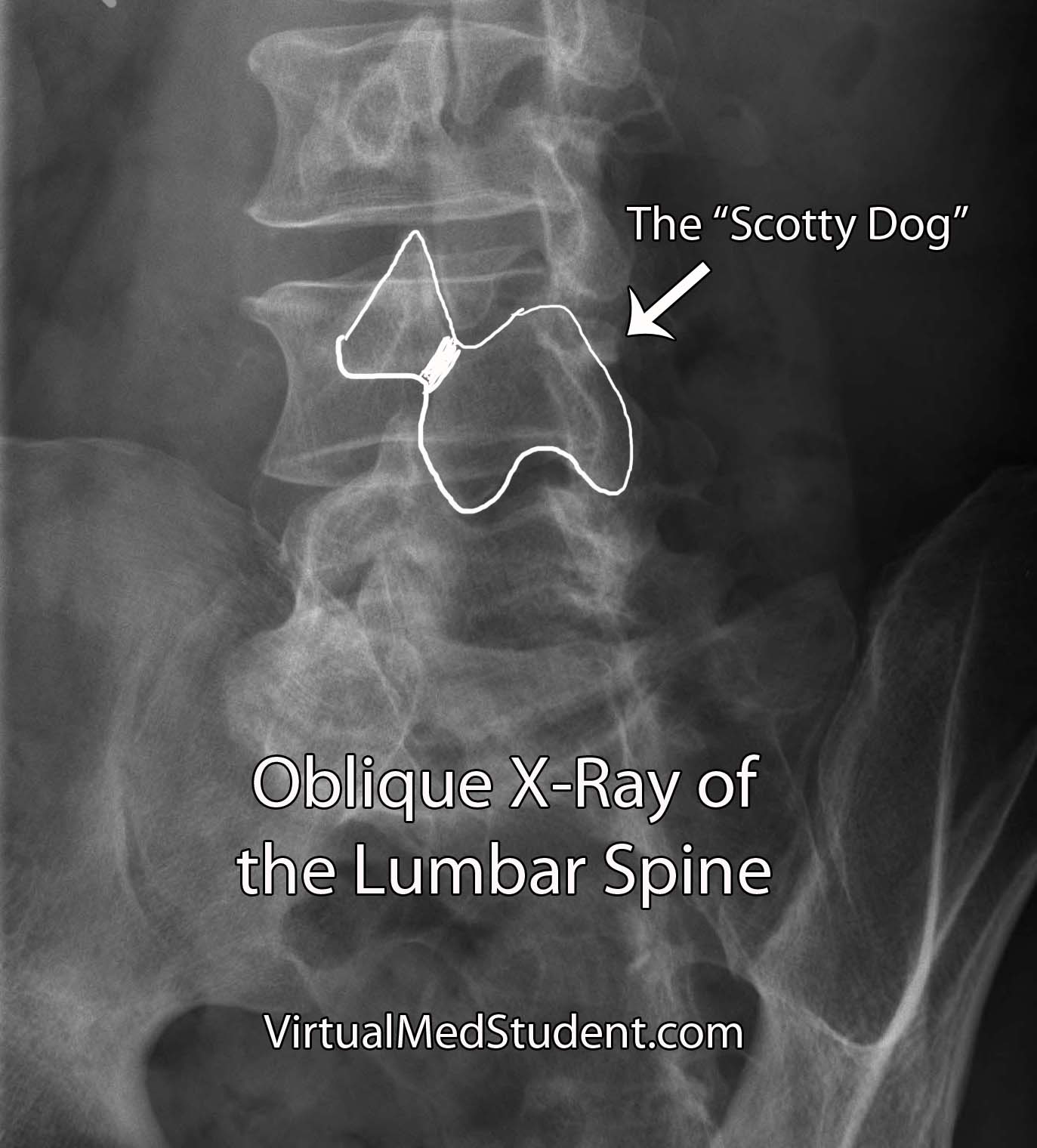
Diagnosis is made by looking at an x-ray or CT scan of the spine. The classic description is a defect through the neck of the “Scotty dog”, which is seen best on an oblique x-ray of the lumbar spine.
What to do About It
Treatment starts with avoidance of the motions that caused the fracture. Occasionally a brace is used to prevent extension of the spine.
Anti-inflammatory medications like ibuprofen are commonly used if pain is significant. After a period of rest, physical therapy can be useful to strengthen muscles and prevent recurrence.
Less commonly surgical repair of the pars defect may be attempted. Surgical candidates are patients who continue to have back pain despite conservative treatment. If the patient receives significant pain relief from pre-operative bupivacaine injection into the defect, then they should be considered excellent surgical candidates.
Overview
Spondylolysis is a defect in the bony pars interarticularis of the vertebrae. It commonly occurs in the lumbar spine after repetitive extension motions. Low back pain is the most common symptom. In the absence of complications like spondylolisthesis treatment is typically conservative and involves bracing, physical therapy, and anti-inflammatories. Diagnosis is made by x-ray and/or CT scan.
For Your Reading Pleasure
- Os Odontoideum: The Floating Bone of the Axis
- Cervical Facet Dislocation: Houston We Have a Problem
- The Hangman’s Fracture
- Latin for Toothlike: Fractures of the Odontoid Process
- Burst Fractures: Axial Loading Leading to Ouch!
- Spondylolisthesis
- Denis’ Three Column Spine: A Simple (Albeit Somewhat Outdated) Way to Think About Spinal Stability
- Ossified Posterior Longitudinal Ligament and Its Clinical Significance
- Atlas Fractures: The Weight of the World on Its Shoulders
If You Need Even More Info
- Sutton JH, Guin PD, Theiss SM. Acute Lumbar Spondylolysis in Intercollegiate Athletes. J Spinal Disord Tech. 2011 Oct 13.
- Leone A, Cianfoni A, Cerase A, et al. Lumbar spondylolysis: a review. Skeletal Radiol. 2011 Jun;40(6):683-700.
- Standaert CJ, Herring SA, Halpern B, et al. Spondylolysis. Phys Med Rehabil Clin N Am. 2000 Nov;11(4):785-803.
- McTimoney CA, Micheli LJ. Current evaluation and management of spondylolysis and spondylolisthesis. Curr Sports Med Rep. 2003 Feb;2(1):41-6.