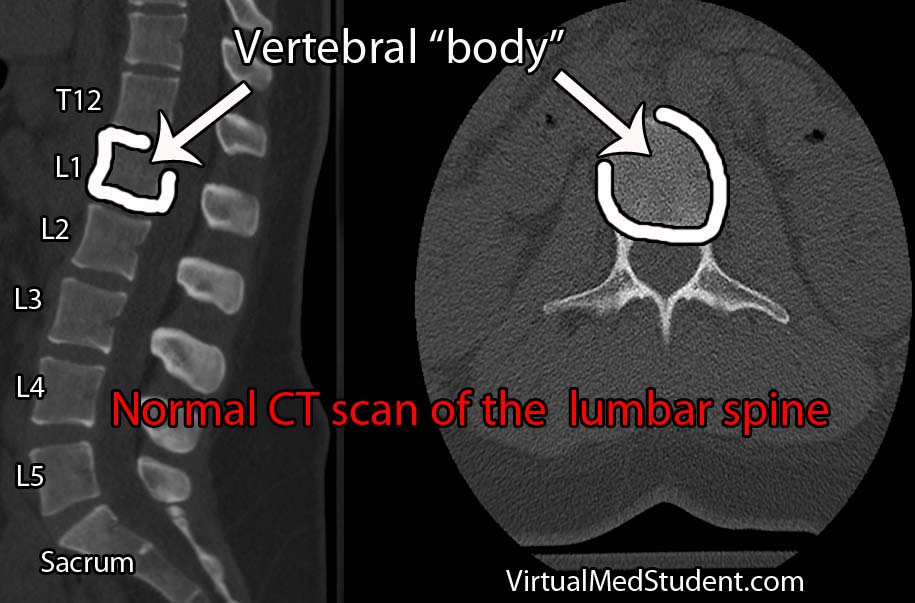
Burst fractures are a specific type of spine fracture in which the body of a given vertebrae “bursts” into pieces. By definition a burst fracture involves the entire vertebral body. The image below is an example of a normal lumbar spine with the vertebral bodies outlined.
Burst fractures most commonly occur at the junction between the thoracic and lumbar spine. This junction is an area where the rigid thoracic spine transitions to the more mobile lumbar spine, and hence is an intrinsic point of weakness. This is why most burst fractures occur between the T10 through L2 vertebrae.
Axial loading of the spine is what causes burst fractures. They typically occur after a traumatic events like car accidents or falls from significant heights. Elderly individuals, and those with poor bone quality, may suffer burst fractures after minor trauma such as falling from a chair.
Signs and Symptoms
Burst fractures invariably present with back pain at the site of the fracture. Depending on the exact location signs and symptoms of nerve root compression or lower spinal cord injury may occur.
If the nerves that dangle in the lumbar spine (aka: the cauda equina) get compressed by the fragments of bone then weakness, numbness, tingling, and even bowel and bladder problems may occur.
Burst fractures between T10 and L1 can cause damage to the end of the spinal cord (the spinal cord ends at L1 or L2 in most individuals), which can lead to lower extremity weakness, or even paralysis, as well as bowel and bladder dysfunction.
Diagnosis
Diagnosis of a burst fracture is made using a combination of x-rays, CT scans, and MRIs. These three imaging modalities serve different functions when evaluating the severity of a burst fracture.
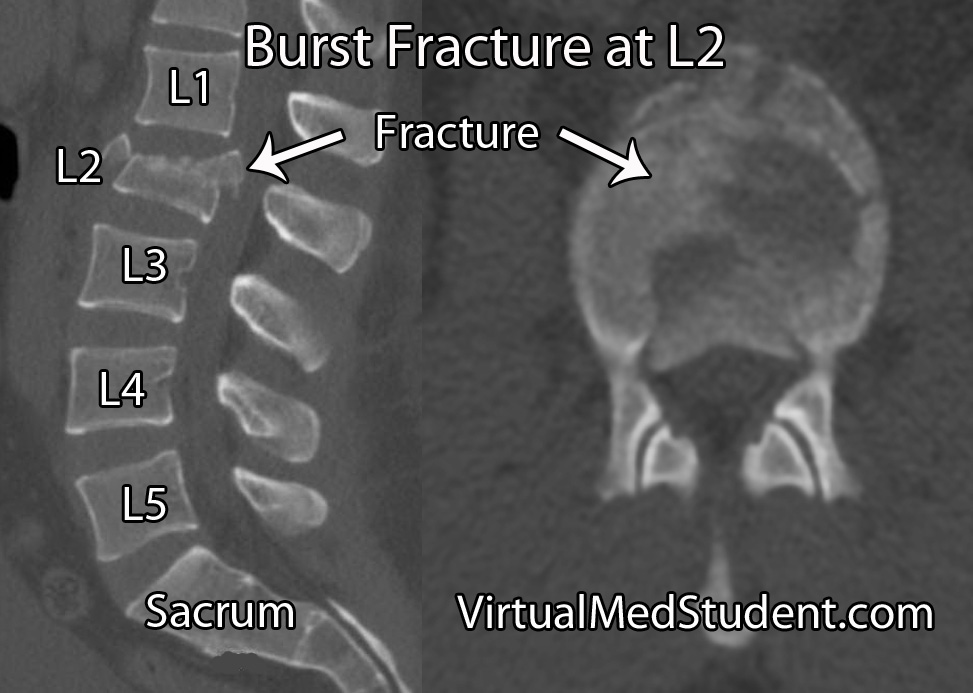
X-rays are usually the first imaging ordered in patients with suspected spine fractures. If the plain x-rays show a burst fracture then CT scanning is usually done to further assess the degree of bony injury (see image below for an example of an L2 burst fracture).
MRI is used to detect ligamentous injury. The degree of ligamentous injury indicates a higher degree of instability; information about ligament integrity helps determine treatment options.
Treatment
Treatment of burst fractures is highly dependent on the severity of the burst fracture. Treatment is either conservative with immobilization in a brace (ie: a "TLSO" or thoracolumbar sacral orthotic brace) or surgical fixation.

- Greater than 50% vertebral body height loss.
- Greater than 25 to 40 degrees of kyphosis.
- Greater than 50% spinal canal compromise.
- Significant posterior ligamentous injury.
- Any neurological signs or symptoms referable to the injury.
- If the patient fails conservative therapy with a brace.
Surgical correction can be achieved in a variety of ways and is often related to surgeon preference. Some surgeons will remove a significant portion of the fractured vertebral body and place a “cage” in the area, a procedure known as a “corpectomy”. This, combined with rods and screws from posteriorly provides the greatest stability, but has a higher risk of nerve injury. Not uncommonly, the fractured vertebral body is left alone and rods and screws are placed from behind only. This is especially true if the fractured level shows minimal spinal canal compromise.
Overview
Burst fractures of the thoracolumbar spine typically occur after high impact axial loading. They usually occur between T10 and L2, but can be seen anywhere in the spine. Patients will almost invariably have pain at the fracture site and may or may not have neurological signs and symptoms depending on the severity of the fracture. Diagnosis is made with CT, plain x-rays, and MRI. Treatment is highly dependent on the individual fracture and ranges from bracing to surgical fixation.
Related Articles
References and Resources
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994 Aug 1;19(15):1741-4.
- Agus H, Kayali C, Arslantas M. “Nonoperative treatment of burst-type thoracolumbar vertebra fractures: clinical and radiological results of 29 patients. Eur Spine J (2005) 14:536-540.
- Denis F. The three column spine and its significance in the classification of acute thoracolumbar spine injuries. Spine (Phila Pa 1976). 1983 Nov-Dec;8(8):817-31.
- Wood K, Butterman G, Mehbod A, et al. Operative Compared with Nonoperative Treatment of a Thoracolumbar Burst Fracture without Neurological Deficit.
- Vaccaro AR, Lehman RA Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005 Oct 15;30(20):2325-33.