Interestingly, cavernous malformations do not have any brain tissue within them. This helps distinguish them from another related vascular abnormality known as an arteriovenous malformation.
The genetics of cavernous malformations have been elucidated by studying familial forms of the disorder. There are at least three known genetic defects that predispose patients to develop cavernomas. These genes appear to be important in the formation of blood vessels (a process known as "angiogenesis") and the blood brain barrier. Therefore, mutations in these genes can cause the abnormal growth of vascular tissue.
What Havock Do These Guys Cause?
Cavernomas can cause numerous signs and symptoms depending on their location within the brain. Seizures are the most common symptom. However, progressive neurological impairment such as worsening weakness can also occur.
Sometimes cavernomas can block the flow of cerebrospinal fluid leading to hydrocephalus. Hydrocephalus can cause increased intracranial pressure leading to headaches, nausea, and vomiting. However, it is important to realize that many patients with cavernomas have no symptoms at all!
If symptoms are present, they tend to progress over time. This is because cavernous malformations bleed and re-bleed resulting in an expansion of its size over time. As the malformation increases in size it can push on adjacent brain tissue causing worsening symptoms.
Unlike arteriovenous malformations, life threatening and severe hemorrhages are rare. Cavernomas bleed at an initial yearly rate of anywhere between 1% to 5%. After the first bleed, the risk of re-bleeding increases to as high as 10% per year. In other words, if a cavernoma bleeds, it is more likely to re-bleed at a later date.
How Do You Diagnose These Buggers?
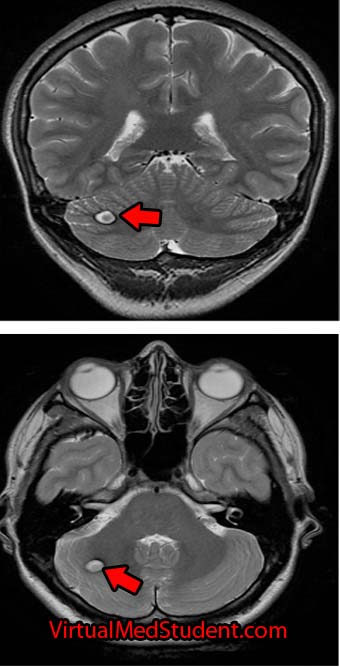
The diagnosis of cavernous malformations are made via imaging studies. They are usually detected via MRIs that are ordered for evaluation of neurological symptoms. Cavernomas are seen best on T2 and gradient echo MRI sequences. They typically look like a piece of popcorn.
Select patients undergo a more invasive imaging procedure known as angiography. Angiography is used to rule out another similar lesion known as an arteriovenous malformation. Since cavernomas are venous malformations they are not seen on angiograms.
How Are These Treated?
Depending on the location, most cavernous malformations in the brain or spinal cord are removed surgically. Some institutions offer radiation as a means of treatment, especially in difficult to access areas (ie: where the risk of surgical removal is very high).
Let’s Recap this MoFo
Cavernous malformations of the brain are abnormal vascular growths composed of capillary networks. They are likely the result of genetic mutations in genes responsible for blood vessel growth. Depending on their location they can cause numerous neurological symptoms such as seizures and weakness. MRI often shows the characteristic “popcorn” lesion. Treatment is usually with surgical resection, although some cavernomas may be radiated depending on their location.
Related Articles
- Colloid Cysts of the Third Ventricle
- Acoustic Neuroma (What We Really Mean is Vestibular Schwannoma
- Hemangiopericytoma: A Tumor of Pericytes
- Hydrocephalus is Greek for “Water Head”
Not Satisfied? More References and Resources…
- Hauptman JS, Moftakhar P, Dadour A, et al. Advances in the biology of cerebral cavernous malformations. Surg Neurol Int. 2010 Oct 11;1:63.
- Li DY, Whitehead KJ. Evaluating strategies for the treatment of cerebral cavernous malformations. Stroke. 2010 Oct;41(10 Suppl):S92-4.
- Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease
. Seventh Edition. Philadelphia: Elsevier Saunders, 2004.
- Greenberg MS. Handbook of Neurosurgery
. Sixth Edition. New York: Thieme, 2006. Chapter 25.
- Nolte J. The Human Brain: An Introduction to its Functional Anatomy
. Sixth Edition. Philadelphia: Mosby, 2008.
- Gross BA, Lin N, Du R, et al. The natural history of cavernous malformations. Neurosurg Focus 30 (6):E24, 2011.