Cervical myelopathy refers to a constellation of signs and symptoms that occur when the spinal cord is squeezed and unable to function properly. Myelopathy is most commonly caused by cervical stenosis, which is a general term used to describe a decrease in the cross sectional area of the spinal canal
Stenosis comes in two flavors: congenital or acquired. In congenital cervical stenosis the spinal canal is developmentally narrower than normal. Congenital stenosis is not considered hereditary, but is present from birth, and is a result of “abnormal” development.
Acquired stenosis is more common, and typically occurs in people over the age of 50. This type of stenosis is caused by a combination of factors and pathologic changes.
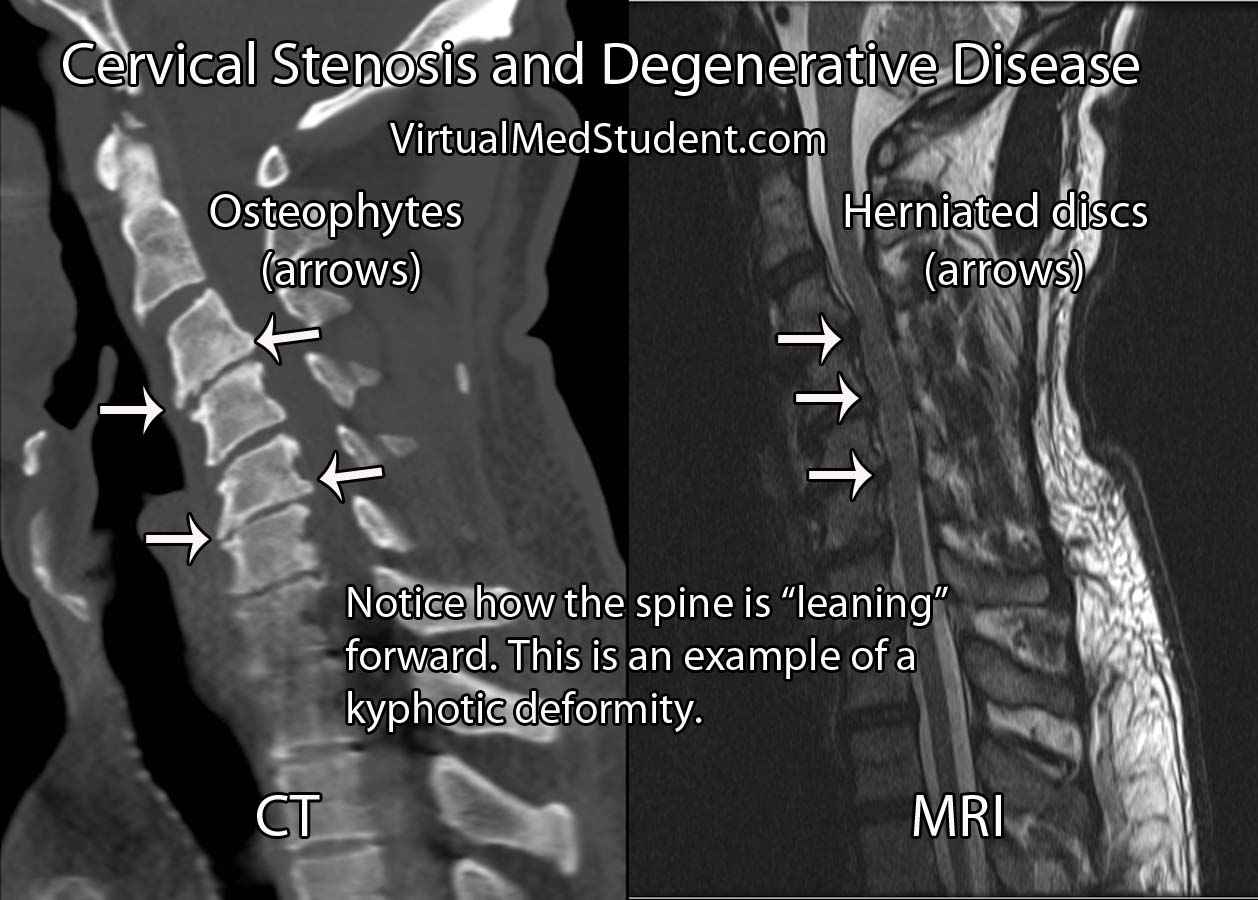
Degenerative cervical disease is the most common cause of acquired cervical stenosis and myelopathy. It has several distinct features, which include: loss of disc height, disc herniation, osteophyte formation, and resultant deformity (ie: kyphosis, or a forward leaning cervical spine). Let’s discuss each of these features in more detail…
The first feature in acquired degenerative stenosis is a loss of intervertebral disc elasticity and height. You can think of the intervertebral discs like shock absorbers for the spinal column. In the cervical spine, a healthy disc is slightly taller at its front most portion and slightly shorter at its back most portion. This gives the normal cervical spine a lordotic curvature.
As someone ages, the discs tend to dry out and the height differential between the front and back of the disc is lost. This can cause the cervical spine to bow forward resulting in a loss of lordosis. The new forward lean to the spine is called a kyphotic deformity. This deformity can cause the cord to stretch over the bones of the spine resulting in myelopathy.
The second factor that contributes to acquired degenerative stenosis is when the back most section of the disc weakens and pooches out towards the spinal cord. This is known as a disc herniation. Disc herniations narrow the cross sectional diameter of the spinal canal and contribute to stenosis.
Finally, as the discs age and dry out they lose their elasticity, and therefore lose their ability to absorb shock. As a result, the bones and ligaments take on more of the burden. They attempt to fight back by forming bony growths known as osteophytes. The osteophytes further narrow the spinal canal and contribute to stenosis.
Let’s bring it all together… Acquired degenerative cervical stenosis occurs when a combination of kyphotic deformity, disc herniations, and osteophytic growths narrow the spinal canal and cause compression of the spinal cord.
Other less common causes of cervical stenosis include ossification of the posterior longitudinal ligament. Additionally, traumatic injuries of the cervical spine can cause immediate cervical stenosis and cord injury. And even less commonly, tumors in the cervical spine can push on the cord and cause stenosis.
It is important to note that cervical stenosis does not always cause myelopathy. In fact, some patients can have a very "tight" cervical cord, but have no signs or symptoms of cord compression.
Signs and Symptoms
Patient’s that are myelopathic present with a constellation of signs and symptoms depending on how "squished" their cord is. Myelopathic patients present with a combination of gait dysfunction, clumsiness when using their hands, weakness, abnormally brisk reflexes, spasticity, and Lhermitte sign.
Signs and Symptoms
of Myelopathy:
– Gait dysfunction
– Clumsiness/weakness
– Brisk reflexes
– Spasticity
– Sensation problems
– Lhermitte’s sign
Patients who have myelopathy tend to walk with a broad based gait as if steadying themselves. They often complain of feeling like they are walking “drunk”. Clumsiness is also a common symptom of myelopathy. Patients will typically complain of problems writing, using a utensil, holding a coffee cup, or performing other fine motor movements.
Finally, a phenomenon known as Lhermitte’s sign can occur. Lhermitte’s sign occurs when someone flexes their head forward and a shock like sensation runs down the neck and back into the extremities. It is a result of compression on the back most portion of the spinal cord, which is an area that relays sensation to the brain.
The Nurick grading system (table below) was designed to assess the severity of myelopathy. It is useful when guiding treatment decisions. The Japanese Orthopedic Association (JOA) score, European Myelopathy Score, Myelopathic Disability Index, and Ranawat Classification are other myelopathy grading scales that are commonly used in clinical practice.
| The Nurick Grading System for Myelopathy | |
| Grade 0 | Nerve root impingement may be present (ie: radiculopathy), but no cord symptoms are present |
| Grade 1 | Able to walk normally, but may have signs (but not symptoms) of cord compression |
| Grade 2 | Some difficulty with walking, but still able to work |
| Grade 3 | Unable to walk to the point of not being able to work |
| Grade 4 | Can only walk when assisted |
| Grade 5 | Confined to a wheelchair or bed bound |
Diagnosis and Classification
Diagnosis of cervical stenosis is based on imaging (ie: CT, MRI, etc). Remember that stenosis does not necessarily translate into myelopathy! Patient’s should be symptomatic as well! A stenotic spine is radiographically present when the diameter of the spinal canal in the antero-posterior plane is less than 10mm.
An alternative way of diagnosing cervical stenosis is using Pavlov’s ratio. This is defined as the ratio of the canal diameter to the diameter of the adjacent vertebral body; any ratio less than 0.8 is worrisome.
Treatment
Treatment of cervical stenosis depends on several factors. First and foremost are symptoms. If a patient is not myelopathic, then frequently the best course of action is to monitor the patient until signs or symptoms of myelopathy appear.
If symptoms are present, the discussion becomes whether or not to reconstruct and decompress the front part of the spine (ie: an anterior approach), the back part of the spine (ie: a posterior approach), or both.
Anterior approaches come in one of two flavors. The first is removal of the disc with placement of a bone graft; this is formally known as a cervical discectomy and fusion. When the bones of the spine are causing the compression a more extensive surgery known as a corpectomy is performed; in this procedure the entire vertebral body is removed and a cage is placed in its place to reconstruct the spine.
Posterior approaches include laminoplasty and laminectomies with or without instrumented fusion. Laminoplasty involves splaying open the lamina so that the spinal cord can drift back. Laminectomies involve un-roofing the bone behind the spinal cord. Laminectomies are frequently done with an instrumented fusion in which rods and screws are placed to help the patient maintain a normal cervical alignment (ie: lordosis).
| Surgical Treatment of Myelopathy | ||
| Deformity | Compression | Surgical Approach |
| Kyphotic | Anterior and only 3 spinal levels or less involved | Anterior (anterior cervical discectomies and/or corpectomies) |
| Kyphotic | Anterior and posterior | Combined anterior (anterior cervical discectomies and/or corpectomies) and posterior (laminectomies with or without instrumented fusion) |
| Lordotic | Anterior and only 3 spinal levels or less involved | Anterior (anterior cervical discectomies and/or corpectomies) |
| Lordotic | Posterior | Posterior (laminoplasty or laminectomies with or without posterior instrumented fusion) |
| Lordotic | Anterior and posterior | Combined anterior (anterior cervical discectomies and/or corpectomies) and posterior (laminectomies with or without instrumented fusion) |
The choice of surgical options is highly dependent on the degree of deformity, instability, and where specifically (ie: what levels) in the spine the cord compression is located.
Ultimately, the surgical treatment of cervical stenosis and myelopathy must be tailored to each individual patient based on many factors.
Overview
Cervical stenosis is abnormal narrowing of the spinal canal. It has numerous causes, of which the most common one is acquired degenerative stenosis. Stenosis can cause compression of the spinal cord, which can cause signs and symptoms of myelopathy. Treatment for symptomatic patients involves decompressing the spinal cord via either an anterior, posterior, or combined approach.
Related Articles
- Ossified posterior longitudinal ligament
- Atlas fractures
- Hangman’s fracture
- Dislocated facet joints (jumped facets)
- Os odontoideum
- Odontoid fractures
- Cauda equina syndrome
References and Resources
- Revanappa KK, Rajshekhar V. Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur Spine J. 2011 Sep;20(9):1545-51.
- Scardino FB, Rocha LP, Barcelos AC, et al. Is there a benefit to operating on patients (bedridden or in wheelchairs) with advanced stage cervical spondylotic myelopathy? Eur Spine J. 2010 May;19(5):699-705.
- Emery SE, Bohlman HH, Bolesta MJ, et al. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. 1998 Jul;80(7):941-51.
- Wada E, Suzuki S, Kanazawa A, et al. Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine (Phila Pa 1976). 2001 Jul 1;26(13):1443-7; discussion 1448.
- Manzano GR, Casella G, Wang MY, et al. A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery. 2012 Feb;70(2):264-77.
- Ranawat CS, O’Leary P, Pellicci P, et al. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979 Oct;61(7):1003-10.
- Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87-100.
- Vitzthum HE, Dalitz K. Analysis of five specific scores for cervical spondylogenic myelopathy. Eur Spine J 2007;16:2096–103.
- Herdmann J, Linzbach M, Krzan M, et al. The European myelopathy score. In: Baucher BL, Brock M, Klinger M, eds. Advances in Neurosurgery. Vol. 22. Berlin, Germany: Springer; 1994:266–8.
- Clark E, Robinson PK. Cervical myelopathy: a complication of cervical spondylosis. Brain. 1956 Sep;79(3):483-510.