Pyogenic liver abscesses are localized collections of pus and bacteria. The initial infection occurs when bacteria travel through the portal vein. This most commonly occurs after bowel contents leak into the peritoneal cavity from the gut. Other causes of liver abscesses include direct spread of infection from the bile duct system, or from other bacterial infections of the blood. Rarely, penetrating injuries (gunshots, stab wounds, surgery) may directly introduce infection. There are numerous “bugs” that can cause pyogenic liver abscesses. They include, but are not limited to, streptococcus species, klebsiella pneumoniae, and staphylococcus species.
Signs and Symptoms
Similar to other infections, liver abscesses can cause fevers, chills, decreased appetite, abdominal pain, and a generalized sense of not feeling well (ie: malaise). Interestingly, hiccups may also be present if the abscesses are causing adjacent inflammation/irritation of the diaphragm.
Diagnosis
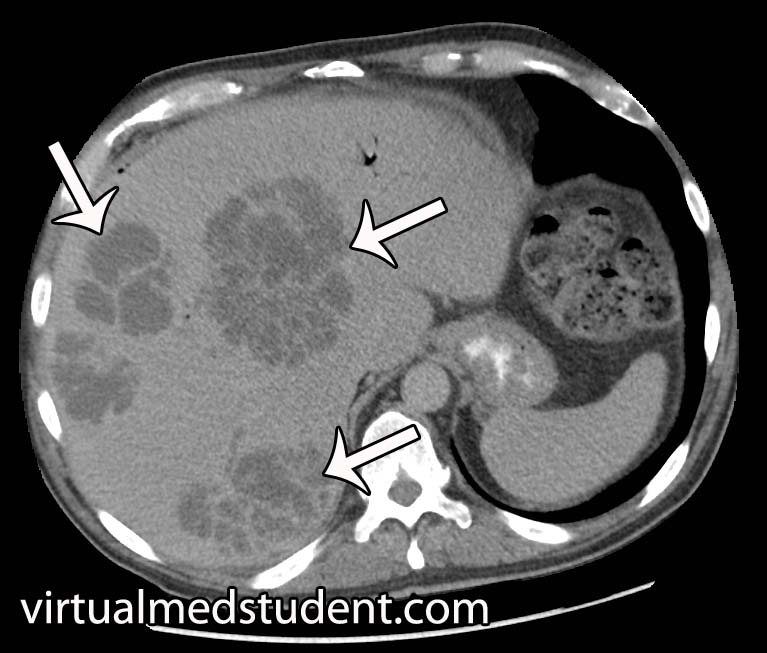
Another commonly employed imaging modality is the use of ultrasound to detect the fluid filled pockets within the liver.
However, it is important to note that imaging studies alone cannot distinguish between the different types of liver abscesses. Imaging can also not tell you what bacteria is responsible for the abscess.
Treatment
Pyogenic abscesses must be drained and treated with antibiotics. Drainage is usually done under image guidance using a needle placed through the skin into the abscess. Although occasionally direct surgical evacuation of the abscess is necessary.
Draining the abscess is important for two reasons. First, it decreases the size of the abscess allowing antibiotic therapy to work more effectively. And secondly, it provides abscess fluid that can be sent to the lab for bacterial culture and gram stain.
The results of the culture help guide subsequent antibiotic therapy. Commonly used antibiotics include piperacillin-tazobactam (Zosyn®), vancomycin, metronidazole (Flagyl®), and ceftriaxone; once cultures confirm the causative bug antibiotic therapy can be narrowed.
Overview
Pyogenic liver abscesses are collections of pus and bacteria. They occur most commonly after the spilling of gut bacteria into the peritoneal space (ie: peritonitis). There are numerous causative bacteria. Symptoms include fever, chills, decreased appetite, and abdominal discomfort. Treatment is with drainage and antibiotics.
References and Resources
- Hasper D, Schefold JC, Baumgart DC. Management of severe abdominal infections. Recent Pat Antiinfect Drug Discov. 2009 Jan;4(1):57-65.
- Benedetti NJ, Desser TS, Jeffrey RB. Imaging of hepatic infections. Ultrasound Q. 2008 Dec;24(4):267-78.
- Mortelé KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004 Jul-Aug;24(4):937-55.
- Kurland JE, Brann OS. Pyogenic and amebic liver abscesses. Curr Gastroenterol Rep. 2004 Aug;6(4):273-9.
