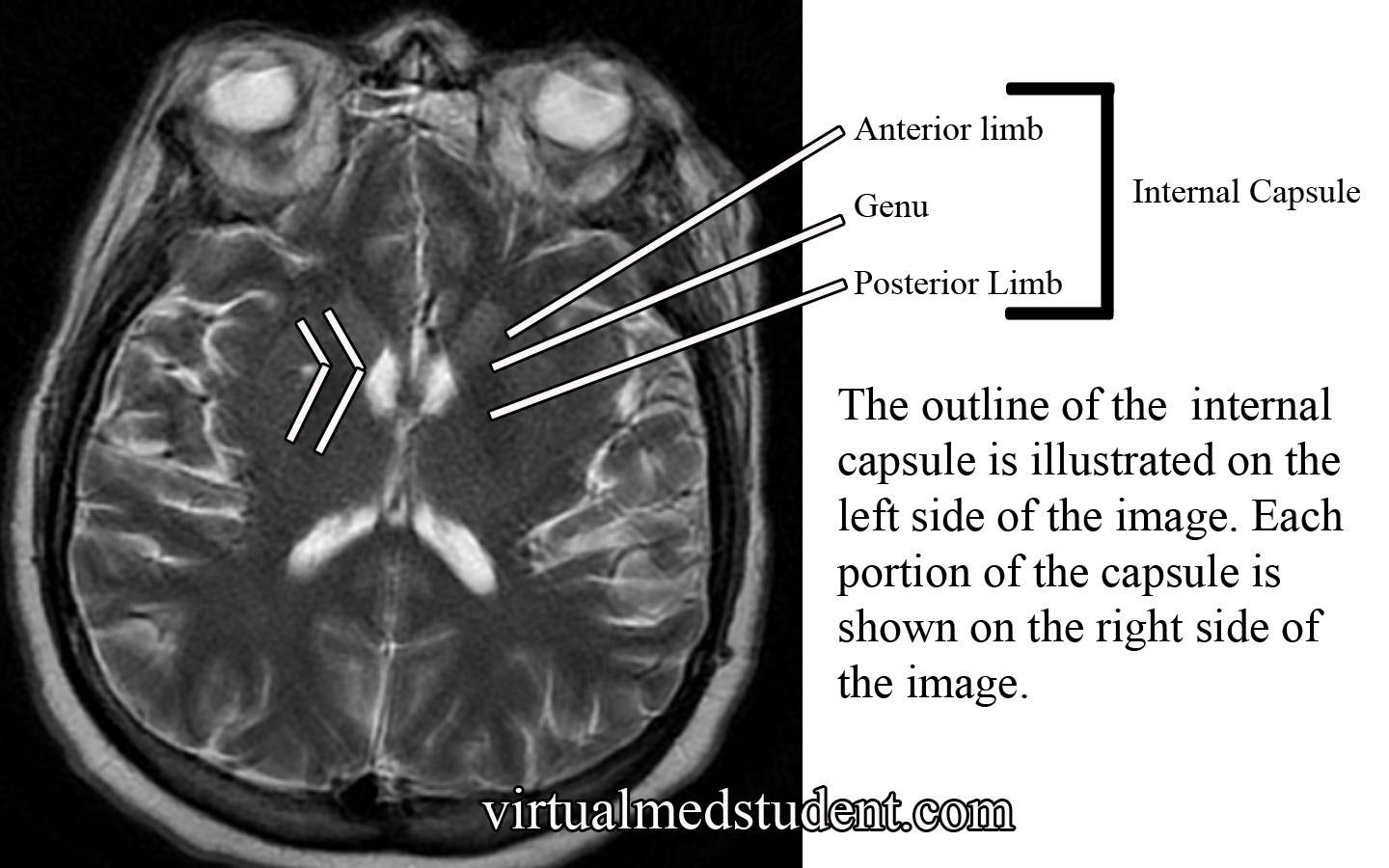
The internal capsule is one pricey piece of brain real estate! It contains all of the pathways that allow information to be transferred between the cerebral cortex and the spinal cord, brainstem, and subcortical structures (ie: thalamus, basal ganglia). It is divided into an anterior limb, posterior limb, and genu (ie: the area where the anterior and posterior limbs meet).
The anterior limb contains axons that send information between the thalamus and the cingulate gyrus and pre-frontal cortex. It also contains axons in the frontopontine pathway (ie: axons going from the frontal cortex to a portion of the brainstem known as the pons).
The genu contains the corticobulbar tract, which originate in the motor areas of the frontal lobes and extend to the cranial nerve nuclei in the brainstem. It also contains axons that connect the motor section of the thalamus (ie: VA and VL nuclei) with the motor areas of the frontal cortex.
The posterior limb contains the corticospinal tract, which are axons that come from the motor area of the frontal cortex and travel all the way to the anterior horns of the spinal cord where α-motor neurons are located. The posterior limb also contains sensory information coming from the body via the medial lemniscus and the anterolateral (aka: spinothalamic tract) systems.
The blood supply to most of the internal capsule comes from the lenticulostriate arteries. These small arteries originate from the first portion of the middle cerebral artery. Two other important arteries also supply portions of the internal capsule: the anterior choroidal artery and the recurrent artery of Heubner. The anterior choroidal artery is a branch of the internal carotid. It supplies the inferior portion of the posterior limb. The recurrent artery of Heubner is a branch of the anterior cerebral artery. It supplies the inferior portions of the anterior limb and the genu.
| Anatomy of the Internal Capsule | ||
| Division | Major Communication Tracts | Blood Supply |
| Anterior limb | – Tracts between the frontal lobe and pons (brainstem) – Tracts between the thalamus and prefrontal cortex – Tracts between the thalamus and cingulate gyrus |
– Lenticulostriate arteries (branches of the middle cerebral artery) – Recurrent artery of Heubner (branch of the anterior cerebral artery) |
| Genu | – Tracts between the motor cortex in the frontal lobe and the cranial nerve nuclei in the brainstem (aka: corticobulbar tract) | – Lenticulostriate arteries (branches of the middle cerebral artery) – Recurrent artery of Heubner (branch of the anterior cerebral artery) |
| Posterior limb | – Tracts between the motor cortex of frontal lobe and anterior horn of spinal cord (aka: corticospinal tract) – Medial lemniscus tract (a continuation of the dorsal columns), which carries information about light touch, vibration, and pressure sensation from the body and spinal cord. – Anterolateral (aka: spinothalamic) tract, which carries pain and temperature information |
– Lenticulostriate arteries (branches of the middle cerebral artery) – Anterior choroidal artery (branch of the internal carotid) |
Importance in Disease

Thalamic intracerebral hematoma
compressing the posterior limb
of the internal capsule
Damage to the internal capsule can be devastating neurologically because it contains so many vital tracts.
For example, a stroke of the anterior choroidal artery can lead to posterior limb damage. This can cause paralysis of the contralateral (ie: opposite) arm and leg secondary to interruption of the corticospinal tract.
Posterior limb disruption can also cause co-existent sensory deficits including an inability to feel light touch, pain, and temperature due to damage of the spinothalamic and medial lemniscal pathways.
Hypertensive hemorrhages in the thalamus or basal ganglia can compress the adjacent fibers of the internal capsule leading to similar clinical findings. The head CT to the right shows a thalamic hemorrhage secondary to severely elevated blood pressure. The patient had compression of the posterior limb of the internal capsule. As a result she was unable to move her left arm and leg, and could not feel pain or light touch on the left side of her body.
Overview
The internal capsule is a vital structure. It contains many communication pathways between the brain’s cortex, brainstem, spinal cord, and subcortical nuclei (ie: thalamus, basal ganglia). Its blood supply comes from branches of the middle cerebral artery (ie: lenticulostriates), anterior cerebral artery (ie: recurrent artery of Heubner), and the internal carotid (ie: anterior choroidal artery). Lesions in this area caused by strokes or hypertensive hemorrhages can have devastating clinical consequences.
Other Pertinent Articles…
References and Resources
- Greenberg MS. Handbook of Neurosurgery. 9th Edition. New York: Thieme, 2006. Chapter 25.
- Chowdhury F, Haque M, Sarkar M, et al. White fiber dissection of brain; the internal capsule: a cadaveric study. Turk Neurosurg. 2010 Jul;20(3):314-22. doi: 10.5137/1019-5149.JTN.3052-10.2.
- Simon RP, Aminoff MJ, Greenberg DA. Clinical Neurology, Seventh Edition (LANGE Clinical Medicine). Seventh Edition. New York: McGraw Hill, 2009.
- Nolte J. The Human Brain: An Introduction to its Functional Anatomy. Sixth Edition. Philadelphia: Mosby, 2008.
- Bickley LS, Szilagyi PG. Bates’ Guide to Physical Examination and History Taking. Ninth Edition. New York: Lippincott Williams and Wilkins, 2007.