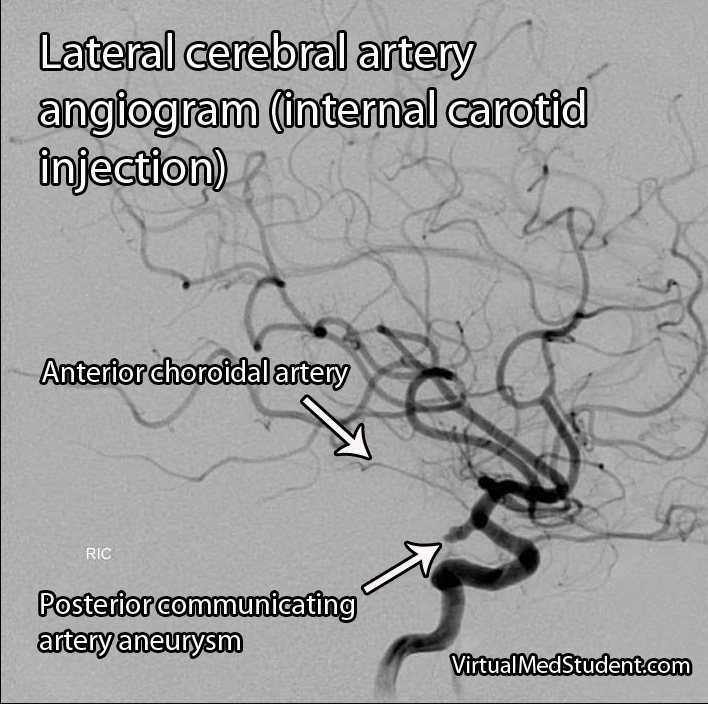
The anterior choroidal arteries are small, but vital blood vessels in the brain. They are branches of the internal carotid arteries. They arise proximal to the splitting of the internal carotid into the anterior and middle cerebral arteries.
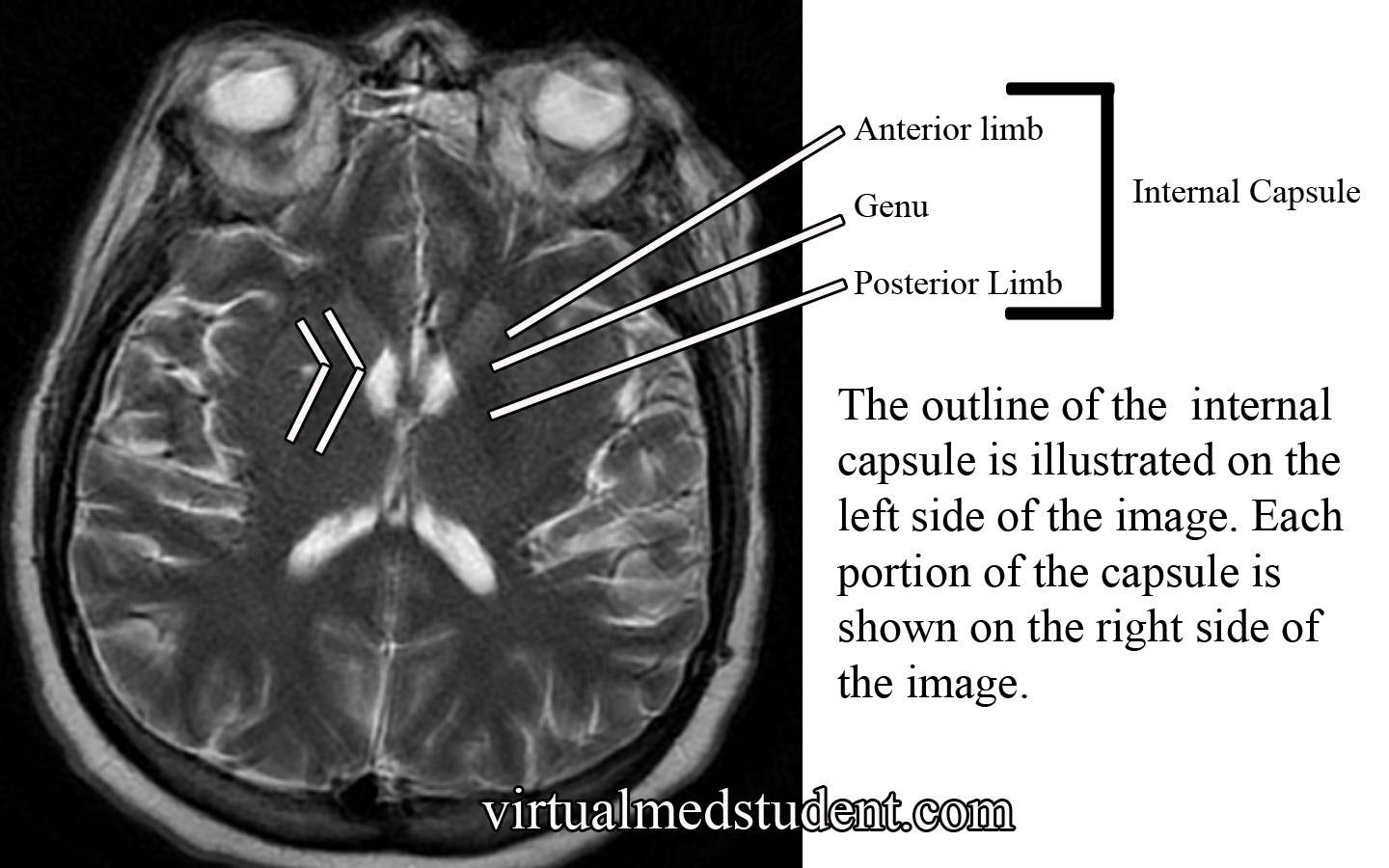
The anterior choroidal arteries deliver blood to vital brain structures. These structures include the posterior limbs of the internal capsules, portions of the thalami, optic tracts, middle third of the cerebral peduncles, portions of the temporal lobes (ie: parts of the pyriform cortex, uncus, and amygdala), substantia nigra, portions of the globus pallidus, as well as the choroid plexus in the lateral ventricles.
The anterior choroidal artery forms connections (anastamoses) with the posterior lateral choroidal arteries. Cerebral angiograms are the best way to visualize the anterior choroidal arteries.
Importance in Disease
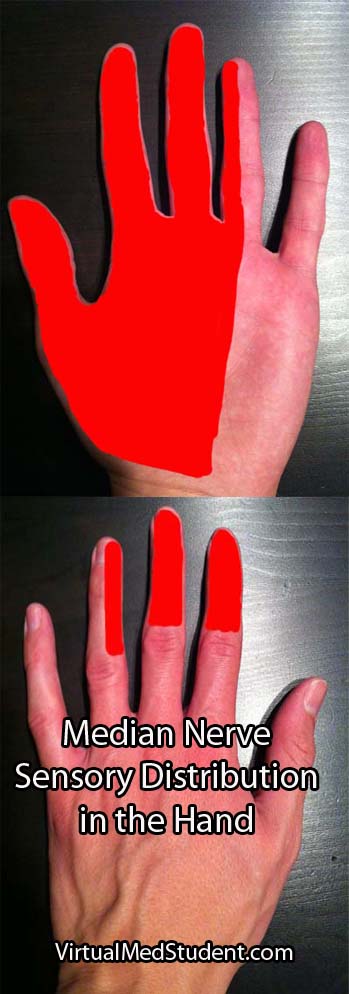
Blockage of the anterior choroidal artery can cause a stroke. The most common symptoms of an anterior choroidal stroke are hemiparesis (weakness on the opposite side of the body), hemianesthesia (decreased sensation on the opposite side of the body), and a homonymous hemianopsia (loss of a portion of the visual field of both eyes). High blood pressure is the most common underlying factor in people with anterior choroidal artery strokes.
The hemiparesis is a result of damage to the posterior limb and genu of the internal capsule. The posterior limb contains the corticospinal tracts, which send information about movement from the brain to the spinal cord.
The hemianesthesia is a result of damage to the ventral posterolateral nucleus of the thalamus. This nucleus contains neurons that receive information from the spinal cord about sensation from the body. This symptom is less common than weakness, and occurs in roughly half of patients with an anterior choroidal stroke.
The final symptom, homonymous hemianopsia, is caused by damage to the optic tracts and lateral geniculate nucleus of the thalamus. Patients lose the ability to see objects on the left or right side (depending on which anterior choroidal artery is involved) in both eyes. This is an even more uncommon symptom, which occurs in less than 10% of patients with an anterior choroidal artery stroke.
Strokes of the anterior choroidal artery rarely cause all three symptoms. This is because the brain tissue served by the anterior choroidals also receives blood flow from other arteries.
Aneurysms of the anterior choroidal arteries are rare and will not be discussed in this article.
Overview
The anterior choroidal arteries are paired structures that arise from the internal carotid arteries. They supply blood to many important structures within the brain. Stroke is the most common pathological disease related to this blood vessel and frequently causes weakness of the opposite side of the body. High blood pressure is the most common underlying disease seen in people who have a stroke in this vascular distribution.
Other Stuff Worth Looking At…
- Hypertension: Understanding and Managing High Blood Pressure
- Internal Capsule: Some Pricey Brain Real Estate
References and Resources
- Pezzella FR, Vadalà R. Anterior choroidal artery territory infarction. Front Neurol Neurosci. 2012;30:123-7. Epub 2012 Feb 14.
- Bruno A, Graff-Radford NR, Biller J, et al. Anterior choroidal artery territory infarction: a small vessel disease. Stroke. 1989 May;20(5):616-9.
- Baehr M, Frotscher M. Duus’ Topical Diagnosis in Neurology: Anatomy, Physiology, Signs, Symptoms. Fourth Edition. Stuttgart: Thieme, 2005.
- Nolte J. The Human Brain: An Introduction to its Functional Anatomy. Sixth Edition. Philadelphia: Mosby, 2008.
- Baskaya MK, Coscarella E, Gomez F, et al. Surgical and angiographic anatomy of the posterior communicating and anterior choroidal arteries. Neuroanatomy (2004) v3:38-42.