
A thrombotic stroke occurs when a blood clot forms in a blood vessel that supplies brain tissue. This is similar to what happens in cardiac infarction (ie: heart attacks). Thrombi are most commonly caused by atherosclerotic disease of the cerebral blood vessels. Thrombi usually form at areas of turbulent blood flow and at locations where vessels form branch points.
Embolic strokes are similar because they are technically blood clots. However, an embolus is a fragment of a clot (thrombus) that formed in another part of the body. Those fragments break free from the original clot and travel to blood vessels in the brain. They get lodged at some point and prevent blood from flowing resulting in a stroke if treatment is not obtained quickly.
Strokes can also be caused by bleeding into brain tissue. These type of strokes are called “hemorrhagic stroke”. Bleeding can occur in people with long standing untreated high blood pressure, or in those that have underlying structural disorders of the blood vessels in the brain (ie: aneurysms or arteriovenous malformations).
Diagnosis
Speedy diagnoses of stroke is extremely important because brain tissue dies quickly if it doesn’t receive adequate oxygen.
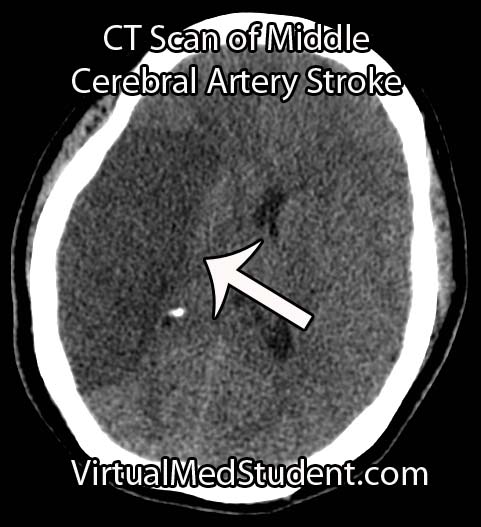
The first test that is done in cases of suspected stroke is a CT scan of the head. The purpose of the CT scan is not necessarily to "see" the stroke, but rather to rule out some other cause (ie: tumor, subdural hematoma, etc) for the symptoms. If bleeding is present on the CT scan the treatment algorithm becomes much different. If no bleeding is seen on CT then the second scan is usually an MRI.
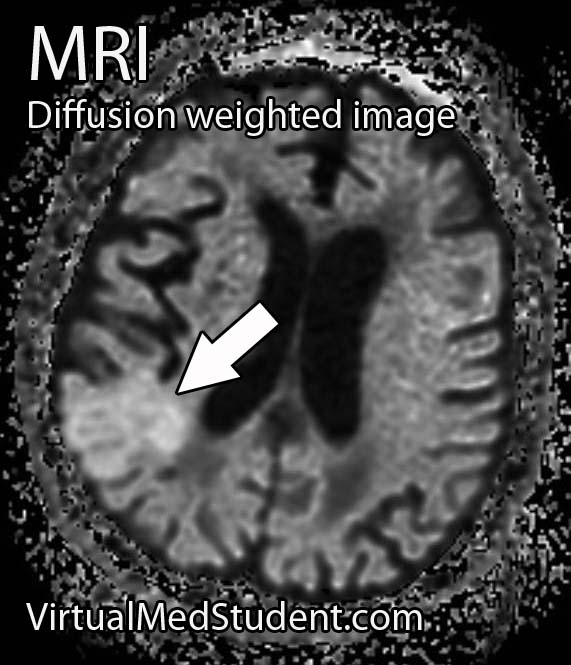
An MRI takes longer than a CT scan, but it gives a much more detailed picture of the brain. In addition, it can pick up ischemia (ie: cell death related to decreased blood flow) much earlier than CT.
The best sequences to detect a stroke on an MRI are the diffusion weighted images and apparent diffusion coefficient maps. Stroked brain tissue will appear “bright” on diffusion weighted imaging and “dark” on the apparent diffusion coefficient map (see images to the left).
In addition, the carotid arteries are scanned using ultrasound in order to detect potential narrowing from atherosclerotic disease. Atherosclerotic carotid arteries are a potential source of emboli.
Sometimes a procedure known as transcranial doppler, which also uses ultrasound technology, is used to detect blood flow in the individual blood vessels of the brain. This can sometimes help determine the specific location of the thrombus/embolus.
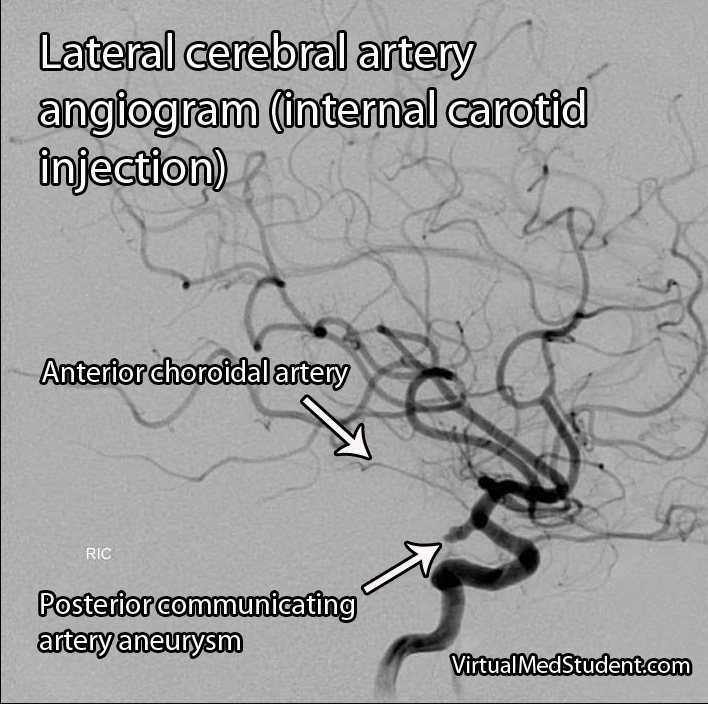
Cerebral angiograms are much more invasive tests, but give a detailed view of which vessels are blocked. Cerebral angiograms can also be used to treat some strokes by directly removing clot from the affected blood vessel.
Most patients should undergo a thorough work up for atherosclerotic disease including a fasting lipid panel and hemoglobin A1C levels (a marker of diabetes).
If the heart is a suspected source of emboli than transthoracic echocardiography (ie: an ultrasound of the heart) is often done as well.
Signs and Symptoms
Cerebrovascular accidents present with a wide variety of signs and symptoms. It is entirely dependent on the blood vessel, and therefore, region of the brain involved. For example, strokes in the left middle cerebral artery will often cause significant language impairments if left untreated. Middle cerebral artery strokes usually cause contralateral paresis as well (usually the face and arm are more affected than the leg). Strokes in the frontal lobes caused by blockage of the anterior cerebral arteries can cause personality changes, as well as paresis/paralysis of the contralateral lower extremity.
Suffice it to say that there are a variety of possible clinical presentations in patients suffering from stroke. These presentations generally correlate with our understanding of brain anatomy and function.
Treatment
Prompt treatment of stroke is critical for preserving viable brain tissue. If a stroke is due to a blood clot (ie: thrombus or embolus) the treatment is with a drug known as tissue plasminogen activator (tPA). tPA is a medication that helps break up the clot.
It can be a dangerous medication because it can cause serious bleeding, but if given early enough, and in the right patient, it can completely prevent brain tissue death. There are numerous contraindications to giving tPA so caution must be used. The traditional teaching is that is should be given within three hours of symptom onset (this is the FDA approved indication); however, up to 4.5 hours from symptom onset has become common in clinical practice (but this is not FDA approved).
Endovascular therapies that mechanically remove the clot are becoming more common, especially for large vessel disease. However, this type of treatment requires specialized interventional neuro-radiologists and is not available in all medical centers. Endovascular therapy with a clot retrieving device is usually indicated up to 6 hours post symptom onset for large vessel occlusions. More distal (ie: further out) occlusions are not candidates for this type of procedure yet.
If a patient survives their first stroke, they are often started on medications to decrease their risk of having a second stroke. One of the most common medications used to prevent a second stroke is aspirin.
However, other medications like ticlopidine and clopidogrel (Plavix®) are also frequently used. All three of these medications prevent platelets (ie: one of the bodies natural ways of forming blood clots) from clumping together. In addition, aspirin is often mixed with another medication called dipyridamole (dipyridamole + aspirin = Aggrenox® in the United States). Patients who have suffered a minor stroke or have high risk transient ischemic attacks should be started on aspirin and clopidogrel and then transitioned to aspirin alone at 21 days.
If atherosclerosis is believed to be the cause of the stroke patients are often started on a statin. This helps slow the process of atherosclerosis and can help prevent another stroke from occurring.
If an embolus was the cause of the stroke patients are often started on an anticoagulant. The most common one used is warfarin (although there are many others). Warfarin is also used to treat a common cause of embolic stroke, an abnormal heart rhythm known as atrial fibrillation.
Overview
Strokes can be caused by thrombi or emboli which are blood clot that block blood flor, or from hemorrhage into brain tissue. Diagnosis is made by CT and MRI scans. Additional studies including carotid ultrasound, cerebral angiography, echocardiography, fasting lipid profiles, and tests for diabetes are also frequently performed.
Treatment depends on the etiology. Tissue plasminogen activator (tPA) is given if thrombi or emboli are the cause, and symptoms began less than 3 hours prior to presentation (4.5 hours is becoming the standard of care). Mechanical endovascular removal of the clot is also possible in some medical centers with specialized equipment.
Prevention of secondary strokes involve the use of anti-platelet (ie: aspirin, clopidogrel), anti-coagulant (ie: warfarin), and anti-atherosclerotic medications depending on the etiology of the previous stroke.
Related Articles
- Atherosclerosis
- Diabetes mellitus
- Hypertension
- Subarachnoid hemorrhage
- Middle cerebral artery stroke
- Monro-Kellie doctrine
- Arteriovenous malformations
- Carotid stenosis
References and Resources
- Amarenco P, Bogousslavsky J, Callahan A, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006 Aug 10;355(6):549-59.
- Barnett HJ, Taylor DW, Haynes RB, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991 Aug 15;325(7):445-53.
- Frontera JA. Decision Making in Neurocritical Care
. First Edition. New York: Thieme, 2009.
- Baehr M, Frotscher M. Duus’ Topical Diagnosis in Neurology: Anatomy, Physiology, Signs, Symptoms
. Fourth Edition. Stuttgart: Thieme, 2005.
- Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998 Nov 12;339(20):1415-25.
- Chambers BR, Donnan GA. Carotid endarterectomy for asymptomatic carotid stenosis. Cochrane Database Syst Rev. 2005 Oct 19;(4):CD001923.
- Gent M, Beaumont D, Blanchard J, et al. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet. 1996 Nov 16;348(9038):1329-39.
- Diener HC, Cunha L, Forbes C. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996 Nov;143(1-2):1-13.
- Diener HC, Bogousslavsky J, Brass LM, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004 Jul 24-30;364(9431):331-7.
- Pan WS, et al. Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack. JAMA Neurology, 2019.