In the upper leg, the sciatic nerve gives off branches to the hamstring muscles. These muscles, which include the semimembranous, semitendinous, biceps femoris and part of the adductor magnus, are powerful flexors of the knee joint.
After sending off branches to the hamstrings, the sciatic nerve hits the back of the knee. At the popliteal fossa the sciatic splits into two distinct nerves: the common peroneal nerve and the tibial nerve.
The first nerve, the common peroneal (aka: common fibular), wraps around the outside of the knee and over the head of the fibula. It then branches into two separate nerves: the superficial peroneal and deep peroneal nerves.
The superficial peroneal nerve innervates two muscles: peroneus longus and brevis (aka: fibularis longus and brevis). These muscles allow you to evert (ie: allow you to lift your "pinky" toe higher than your "big" toe) and plantarflex (ie: help you step on the gas pedal) the foot. This nerve also provides the sensation to the outside half (ie: lateral half) of the lower leg, as well as the top of the foot.
The deep peroneal nerve innervates three muscles in the leg: tibialis anterior, extensor digitorum longus, and extensor hallucis longus. Tibialis anterior allows you to dorsiflex (ie: lift your foot off the ground) and invert (ie: bring your "big" toe higher than your "pinky" toe) your foot. Extensor digitorum longus helps you extend your toes (ie: the opposite of curling them), as well as evert, and dorsiflex your foot. The third muscle, extensor hallucis longus allows you to extend your big toe.
The deep peroneal nerve also innervates two muscles in the foot: extensor digitorum brevis (also helps to extend the toes) and extensor hallucis brevis (also helps to extend the big toe).
| Peroneal Nerve and its Branches | |
| Branch | Muscles |
| Superficial peroneal | – Peroneus longus – Peroneus brevis |
| Deep peroneal (leg branches) |
– Tibialis anterior – Extensor digitorum longus – Extensor hallucis longus |
| Deep peroneal (foot branches) |
– Extensor digitorum brevis – Extensor hallucis brevis |
The other branch of the sciatic nerve, the tibial nerve, dives deep into the lower part of the leg where it acts on muscles in the calf and foot. In the calf it innervates the gastrocnemius (commonly called the "calf" muscle), soleus, popliteus, plantaris, flexor digitorum longus, flexor hallucis longus, and tibialis posterior. The gastrocnemius, soleus, and tibialis posterior are important plantarflexors of the foot (ie: allow you to "step on the gas pedal"). Flexor digitorum longus and flexor hallucis help flex (ie: curl) the toes.
The tibial nerve also sends branches into the foot. It further branches into the medial plantar and lateral plantar nerves, which innervate numerous muscles (see table below) in the foot itself.
The tibial nerve branches in the foot, namely the medial plantar and lateral plantar nerves also provide sensation to the sole of the foot.
| Tibial Nerve and its Branches | |
| Branch | Muscles |
| Tibial nerve (leg branches) | – Gastrocnemius – Soleus – Popliteus – Plantaris – Flexor digitorum longus – Flexor hallucis longus – Tibialis posterior |
Tibial nerve (foot branches) -> medial plantar nerve |
– Abductor hallucis – Flexor digitorum brevis – First lumbrical |
| Tibial nerve (foot branches) -> lateral plantar nerve |
– Flexor digiti minimi – Adductor hallucis – Interossei – 2nd, 3rd, 4th lumbricals – Abductor digiti minimi |
Importance in Disease
The most well known problem of the sciatic nerve is a condition termed "sciatica". Sciatica is not a disease or disorder in itself, but rather a symptom of some underlying spine or nerve pathology. It is most often due to compression of one or more of the nerve roots that contribute axons to the sciatic nerve (L4-S3).
Compression of the nerve roots can be caused by many different pathologies, of which the most common is a herniated disc. Other causes include spinal stenosis and spondylolisthesis. Rarely, the nerve itself is compressed at some point as it travels down the leg.
A common symptom of sciatica is a severe and sharp pain that starts in the lower back and shoots down the buttock and back of the leg. If the involved nerve roots are severely compressed, weakness may also occur. This can cause a "foot drop" (ie: an inability to lift your foot off the ground).
The sciatic nerve may also get compressed as it passes through the piriformis muscle in the pelvis. When this occurs weakness of the hamstrings, lower leg, and foot muscles occurs; in addition, sensation of the outside of the lower leg, the calf, and the sole of the foot may also be affected.
Overview
The sciatic nerve is really two nerves that split at the level of the knee. The two main branches are the common peroneal (aka: common fibular) and tibial nerves, each of which branch again to innervate different muscles in the lower leg and foot. The most common pathologic problem with the sciatic nerve is a constellation of symptoms termed "sciatica". Sciatica is caused, most commonly, by compression of the nerve roots (L4-S3) in the spine that give rise to the sciatic nerve.
More Anatomy You Should Know…
- Peroneal nerve
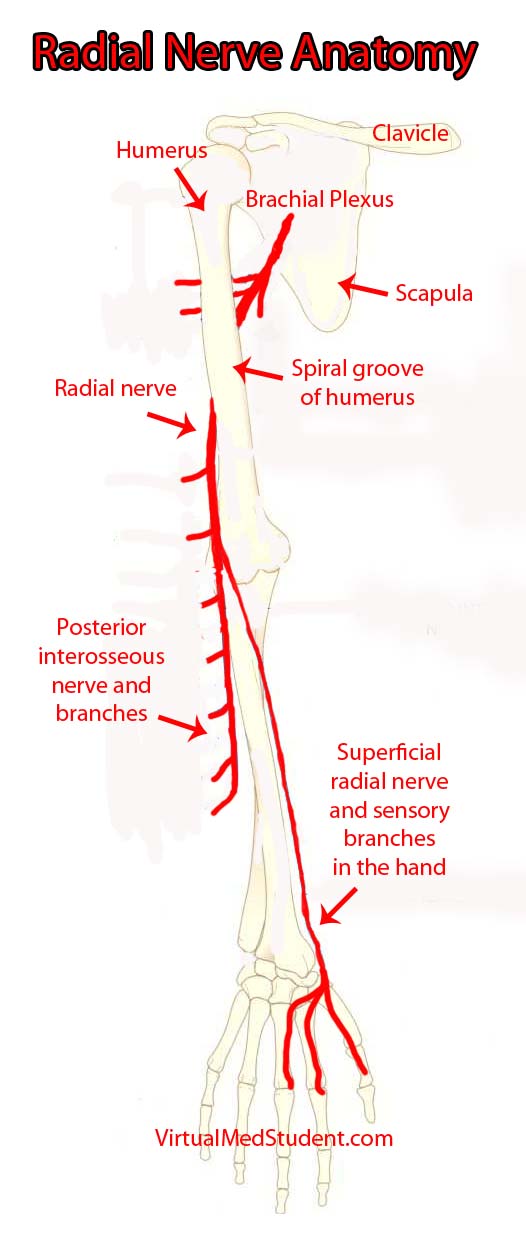
- The Radial Nerve and the Saturday Night Palsy
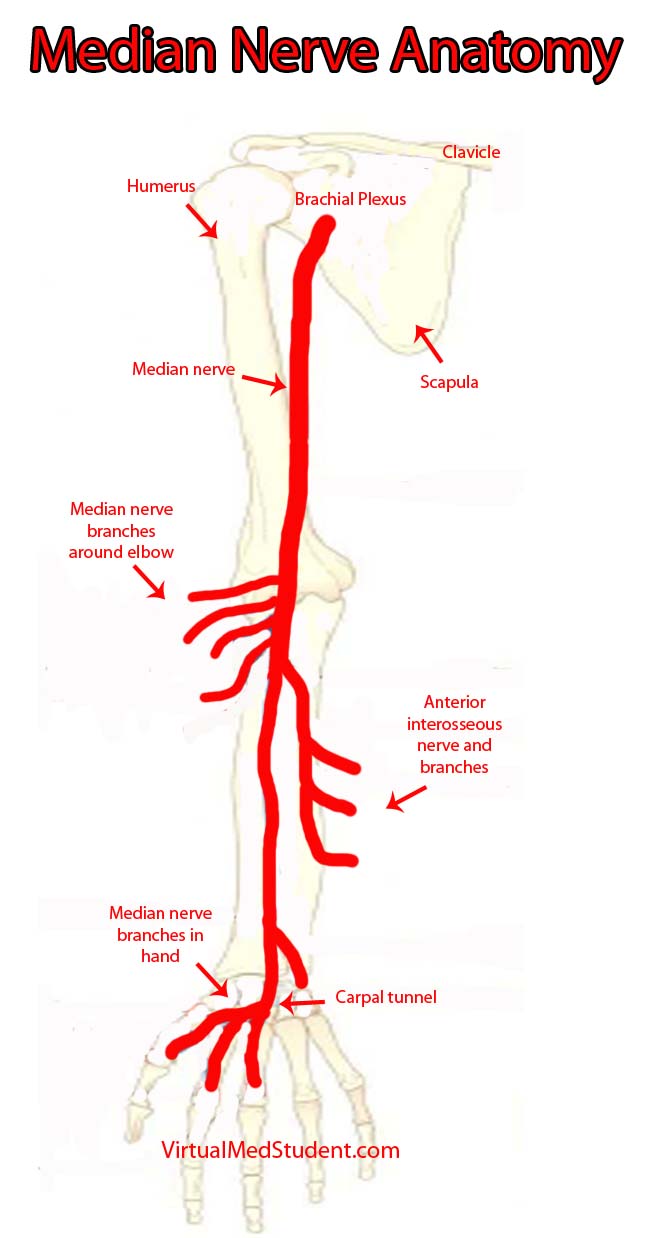
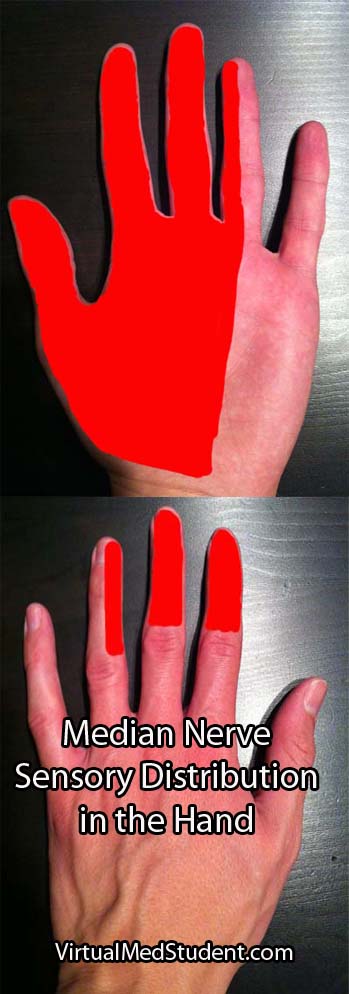
- The Median Nerve: Anatomy, Function, and Clinical Significance
- Cauda Equina Syndrome: Pee, Poop, and Leg Problems
References and Resources
- Greenberg MS. Handbook of Neurosurgery
. Sixth Edition. New York: Thieme, 2006. Chapter 25.
- Prakash, Bhardwaj AK, Devi MN. Sciatic nerve division: a cadaver study in the Indian population and review of the literature. Singapore Med J. 2010 Sep;51(9):721-3.
- Yuen EC, So YT. Sciatic neuropathy. Neurol Clin. 1999 Aug;17(3):617-31, viii.
- Simon RP, Aminoff MJ, Greenberg DA. Clinical Neurology, Seventh Edition (LANGE Clinical Medicine)
. Seventh Edition. New York: McGraw Hill, 2009.
- Netter FH. Atlas of Human Anatomy: with Student Consult Access (Netter Basic Science)
. Fifth Edition. Philadelphia: Saunders Elsevier, 2010.
- Bickley LS, Szilagyi PG. Bates’ Guide to Physical Examination and History Taking
. Ninth Edition. New York: Lippincott Williams and Wilkins, 2007.